Wisdom Teeth Removal (What’s Involved?)
Wisdom teeth removal is a daunting procedure that most people fret about in their early years.
According to a recent study, 10 million wisdom teeth are removed from 5 million patients every year.
It’s stressful to think about being put to sleep, having teeth extracted, and managing the pain after; while bedridden for days.
Understanding the wisdom teeth removal process from start to finish will help eliminate fear, anxiety, and worry before surgery.
Need Dental Advice? Ask Dr. Hannan!
What Are Wisdom Teeth?
Wisdom teeth or third molars are the last adult teeth to erupt and are located in the back of the mouth.
They come in between the ages of 17 and 25, but their eruption time is variable. Most people have four wisdom teeth (two on top and two on the bottom); however, it’s possible to have one, two, three, or more than four; the extra teeth are called supernumerary teeth.
They are called wisdom teeth because they come in when you are more mature in age. Because wisdom teeth are the last teeth to erupt, there is minimal room left in the mouth for them to fit.
Occasionally they can fit without any issues; often, they need to be removed because of lack of space, impaction (poor tooth position), gum issues, or cavities.
Is It Necessary to Remove Wisdom Teeth?
No, it’s not necessary to remove all wisdom teeth.
This question has been debated for many years within the dental community whether or not wisdom teeth should be prophylactically removed, referring to the removal of wisdom teeth to prevent future problems.
Although wisdom teeth removal is highly successful, potential adverse effects can occur, such as pain, soreness, prolonged numbness, or permanent numbness (paresthesia).
The risk of future disease requiring the removal of wisdom teeth in patients who don’t have them removed exceeds 70% after 18 years.
Often, a toothache in the back of the mouth or lower jaw is the first sign of wisdom teeth eruption.
Earaches and headaches may also occur due to insufficient space for the wisdom teeth to erupt. This sensation is called referred pain because the pain triggers a response away from the actual pain source.

Common Symptoms
- Toothache
- Gum inflammation
- Cheek biting
- Jaw tenderness
- Difficulty opening and closing
- Food-trap behind 2nd molars
When wisdom teeth erupt and push through the gums, small holes develop and allow food to pack in hard-to-clean areas.
If the food is not cleared away, cavity-causing bacteria will congregate and cause tooth decay.
In addition, gum inflammation will occur, and gum disease and bone loss will occur if left untreated.
Recommended Reading: Wisdom Teeth Pain: Symptoms, Causes, Relief & Home Remedies (Helpful Tips)Although wisdom teeth pain closely resembles TMJ pain or pain caused by a cavity, there are distinct differences. Your dentist will evaluate your teeth and take x-rays; however, these are the most common symptoms of cavity-causing pain.
Cavity Symptoms
- Sensitivity to hot and cold
- Pain when biting down
- Pain caused by a stimulus
- Tooth discoloration
- Visible hole in tooth
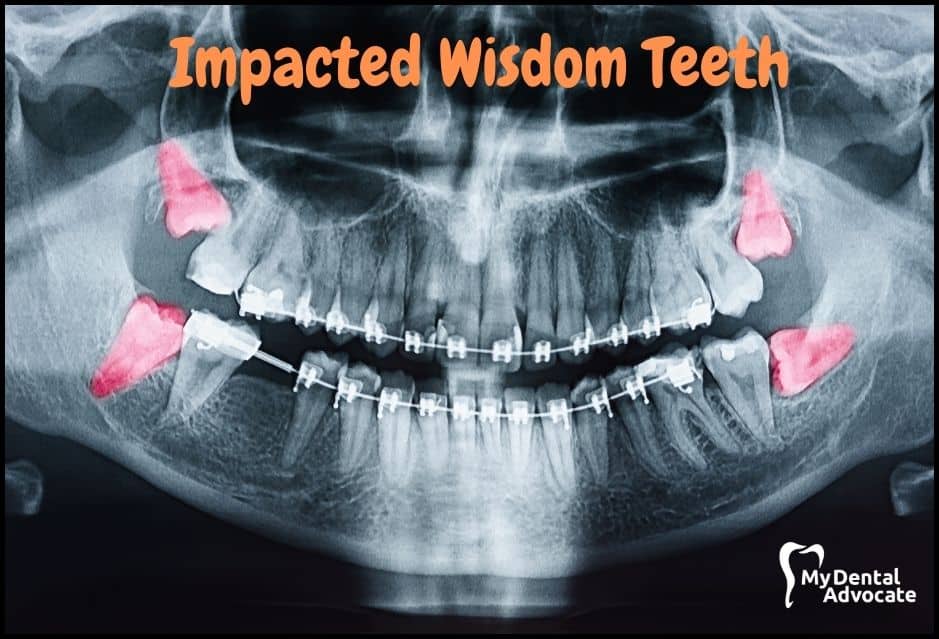
What Are Impacted Wisdom Teeth?
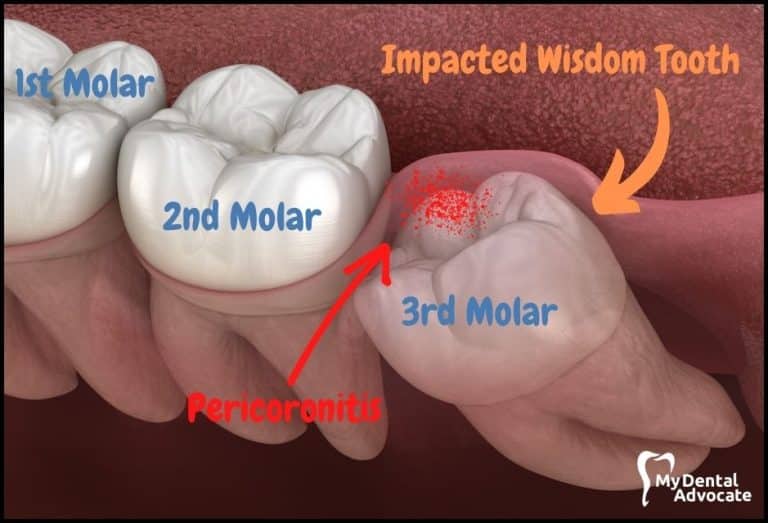
Third molars are impacted when they don’t have enough room to erupt correctly.
These teeth are “stuck” below the bone or gum line and are often positioned sideways toward the adjacent teeth. Impacted wisdom teeth should be extracted before the roots have fully formed, between the ages of 15 and 25.
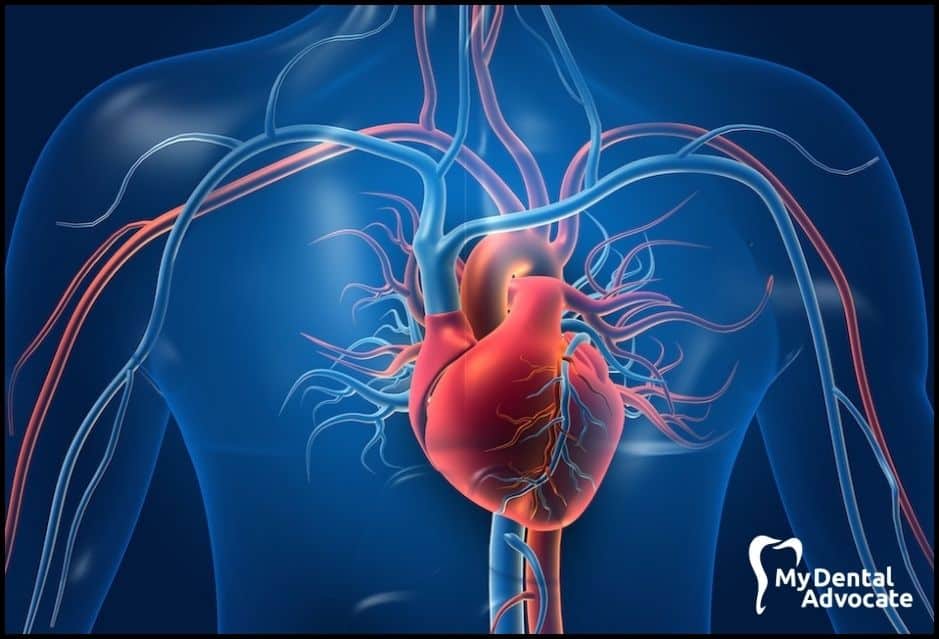
Recommended Reading: Impacted Wisdom Teeth: Symptoms, Causes, Removal & RecoveryUntreated impacted wisdom teeth will harbor bad bacteria. Oral bacteria can travel from your mouth through the gum tissue and into the bloodstream leading to systemic infections affecting the heart, kidneys, and other organs.
Diabetes, heart disease, and kidney disease are common systemic health conditions associated with oral bacteria invasion.
In addition, problems can occur when the roots are fully grown and cause difficulties for the surgeon during the procedure.
Recommended Reading: Dental Opioid Crisis: Understanding the Problem and Practical Solutions9 out of 10 people have at least one impacted wisdom tooth.
Problems Associated with Impacted Wisdom Teeth
- Infection Risks: Improperly erupted wisdom teeth can cause gum irritation, leading to pain and infection (pericoronitis), especially in smokers. A study found 72.4% of 20-25-year-olds experienced pericoronitis before wisdom tooth removal.
- Crowding Concerns: There’s debate among dentists about wisdom teeth causing crowding. While they may contribute, other factors like gum health and tooth shape also play a role.
- Tooth Decay: Crooked wisdom teeth are hard to clean, promoting cavity-causing bacteria. Cavities can form deep below the gum line, making them hard to treat.
- Cyst Formation: Impacted wisdom teeth can lead to jaw cysts, which are difficult to manage and can damage teeth, gums, bone, nerves, and blood vessels.
- Damage to Adjacent Teeth: Wisdom teeth growing towards neighboring teeth can cause tooth resorption, damaging both teeth and often requiring extraction.
- Bone Loss/Periodontal Disease: Impacted wisdom teeth can lead to bone loss around adjacent teeth, potentially necessitating removal if support is inadequate.
Studies have found that periodontal disease in expectant mothers may be associated with a greater likelihood of preterm and low birthrate babies.
When to Remove Wisdom Teeth
Patients are first evaluated by their dentist or orthodontist in their mid-teenage years using oral examination and x-rays to monitor the eruption status of wisdom teeth. Studies show that early detection and treatment intervention provides the best opportunity for success.
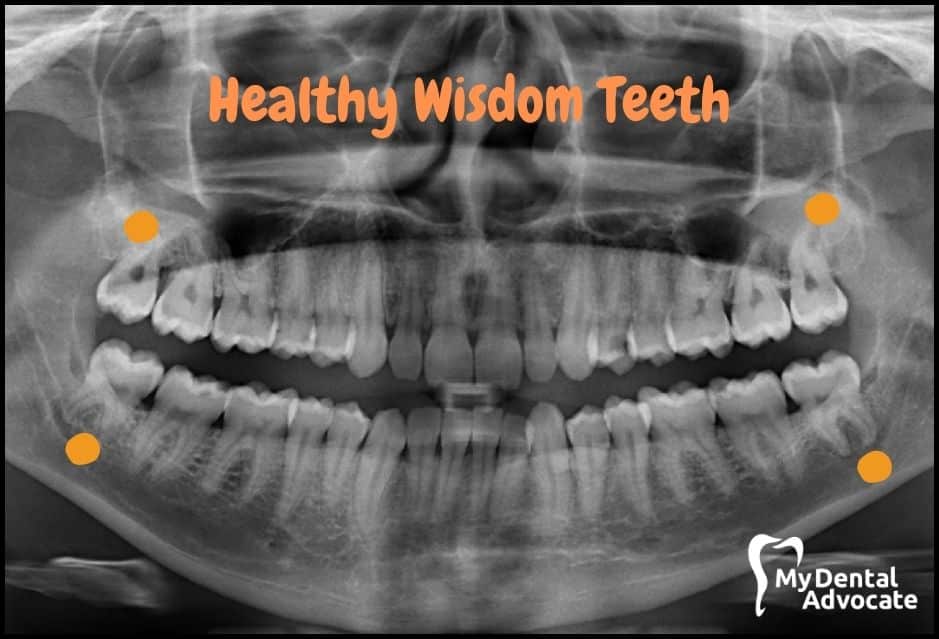
Factors to Retain Teeth
- Completely erupted
- Functional
- Painless
- Cavity-free
- Disease-free
- Healthy & clean
Wisdom teeth are easier to remove when the patient is younger because the roots haven’t fully formed, the bone is softer, and the wisdom teeth are away from nearby nerves and other structures.
In addition, younger patients can recover faster compared to older patients.
Morbidity associated with wisdom teeth extraction and the risk of complications has been shown to increase with age.
On the other hand, wisdom teeth are more difficult to remove the more senior the patient becomes; bone is thicker and denser, and tooth roots extend toward the nerve and other vital structures.
In rare situations, the tooth roots can wrap around the nerve.
First Signs of Wisdom Teeth Eruption
- Inadvertent cheek biting
- Dull ache in the lower jaw
- Jaw is warm to the touch
- Gum tissue is red and inflamed
- White spots on gums
What Is Evidence-Based Management of Third Molars?
Evidence-based clinical decision-making (EBCD) is a systemic approach utilized by clinicians that considers the best available scientific evidence, clinical expertise, and patient values to solve a clinical problem (wisdom teeth extraction).
Evaluating Third Molars Surgery Using (EBCD)
- Every patient & treatment case is unique
- Consider patients’ medical & dental history
- Intraoral & extraoral evaluation
- Radiographic (x-ray) evaluation
- Consultation between dentist, orthodontist, and oral surgeon
- Evaluate pros & cons
Third Molar Treatment Options
According to the American Association of Oral and Maxillofacial Surgeons (AAOMS), “…third molar teeth [with] disease, or are at high risk of developing disease, should be surgically managed. Active clinical and radiographic surveillance is indicated in the absence of disease or significant risk of disease.”
Extraction of third molars reduces the risk for periodontal disease in young adults.
Even though most patients will need their third molars extracted, some patients are able to maintain these teeth for a lifetime with no issues. Yearly intraoral, extraoral, and radiographic (x-ray) observation is recommended for patients with healthy, asymptomatic, disease-free wisdom teeth.
Depending on the consultation results and patient examination, the oral surgeon may extract the tooth, partially remove the tooth or monitor the tooth over time (active surveillance).
It’s important to remember that an absence of symptoms does not equate to a lack of disease.
Key Features
- Extract Tooth: This involves removing the entire tooth, including roots. It’s done when there’s clear access and the roots aren’t near nerves or other tissues.
- Partial Extraction (Coronectomy): Only the tooth’s crown is removed, leaving the roots in the jaw. Ideal when roots are near or entwined with nerves. Post-procedure, roots remain in the bone, but yearly X-rays are advised to monitor their health.
- Active Surveillance: Yearly monitoring of wisdom teeth is essential, especially when they’re asymptomatic, healthy, and have room to erupt. No immediate surgery is needed, but future issues like decay or infection may require intervention.
Wisdom Teeth Classifications
Wisdom teeth classifications are used to predict surgical difficulties and potential complications. In addition to evaluating the position of the third molars, your oral surgeon will factor your age, sex, systemic health, dental health, current medications, and cardiovascular health.
Although there are various classification methods, the most common method is based on the nature of the overlying tissue.
- Erupted: The wisdom tooth is fully visible above the bone and gum. This happens when there’s enough space and the tooth emerges upright.
- Soft Tissue Impaction: The tooth is above the bone but under the gum, not visible in the mouth but may cause a noticeable gum bump. This type is the easiest to remove surgically.
- Hard Tissue (Bony) Impaction: The tooth is stuck below the bone, preventing eruption. It’s categorized into partial or complete bony impaction.
- Partial Bony Impaction: Part of the tooth is above the bone but under the gum. Removal might require cutting the tooth into pieces.
- Complete Bony Impaction: The tooth is entirely trapped, either by its angle or being encased in bone. These are the hardest to remove, often involving significant bone removal and tooth sectioning.
Wisdom Teeth Pain Relief
If you are dealing with wisdom tooth pain there are various methods to help alleviate the pain.
However, it’s best to contact your dentist as soon as possible for an evaluation. In the meantime, over-the-counter medication such as Ibuprofen or Tylenol will help alleviate pain and inflammation.

Pain Relief Methods
- Saltwater rinse
- Topical benzocaine
- Clove oil
- Cold compress
- Antibiotics
Sedation Options for Wisdom Teeth Removal
Most patients and clinicians prefer sedation during third molar extractions to relieve patient anxiety and minimize unexpected movements that could compromise the surgical procedure.
In addition, sedation will suppress the patient’s stress level, preventing a spike in blood pressure that may lead to a cardiovascular event (heart attack).
Recommended Reading: Sedation Options for Wisdom Teeth Removal (Read this FIRST)If the wisdom teeth are erupted and easily accessible to the surgeon, local anesthesia can be administered without sedation for surgical extractions.
However, sedation dentistry is advised for most wisdom teeth if the patient is between the ages of 15 and 25 because the teeth are impacted and require more extensive surgical treatment.
Aside from nitrous oxide (laughing gas), the two most common sedation methods are conscious sedation and general anesthesia (deep sedation).
Methods
- Nitrous Oxide (Laughing Gas): Quick to take effect and wear off, this gas keeps you calm and comfortable but awake and responsive. You won’t need a designated driver afterward.
- Oral Conscious Sedation: Commonly using Valium, this involves taking a pill 30-60 minutes before your appointment. You’ll be monitored in the office and need someone to drive you home, as you might not remember the visit.
- IV Conscious Sedation: Stronger and faster-acting than oral sedation, it’s administered via IV. You can still respond during the procedure but likely won’t recall it. A designated driver is required for your trip home.
- General Anesthesia: Often used for wisdom teeth removal, it puts you to sleep during the procedure. Your vitals are closely watched, and you’ll wake up afterwards without any memory of the dental work.
What’s Involved BEFORE Wisdom Teeth Extractions?
If your dentist or orthodontist recommends removing your wisdom teeth, they will refer you to an oral surgeon (OMS) for the procedure.
The surgeon will review your medical and dental history, current medications, and other information during your consultation appointment.
Recommended Reading: 10 SIMPLE Steps to Prepare for Wisdom Teeth SurgeryIn addition, the surgeon will review your x-rays and discuss the treatment plan and what to expect. This is a great time to ask any question you believe is helpful before the procedure. Ultimately, your surgeon desires you to be comfortable and understand what’s involved.
What’s Involved DURING Wisdom Teeth Extractions?
On the day of your surgery, it’s essential that you don’t eat or drink 8 hours before the procedure, although the dentist will advise you to take medication you generally take (unless it interferes with the procedure – your surgeon will discuss this with you).
Generally, wisdom teeth can be extracted with little to no pain, and the procedure will take 30-60 minutes to complete. Plan accordingly, as you and your driver will be in the office for approximately 90 minutes.
Wisdom teeth extractions are considered an outpatient procedure, so you can go home afterward.
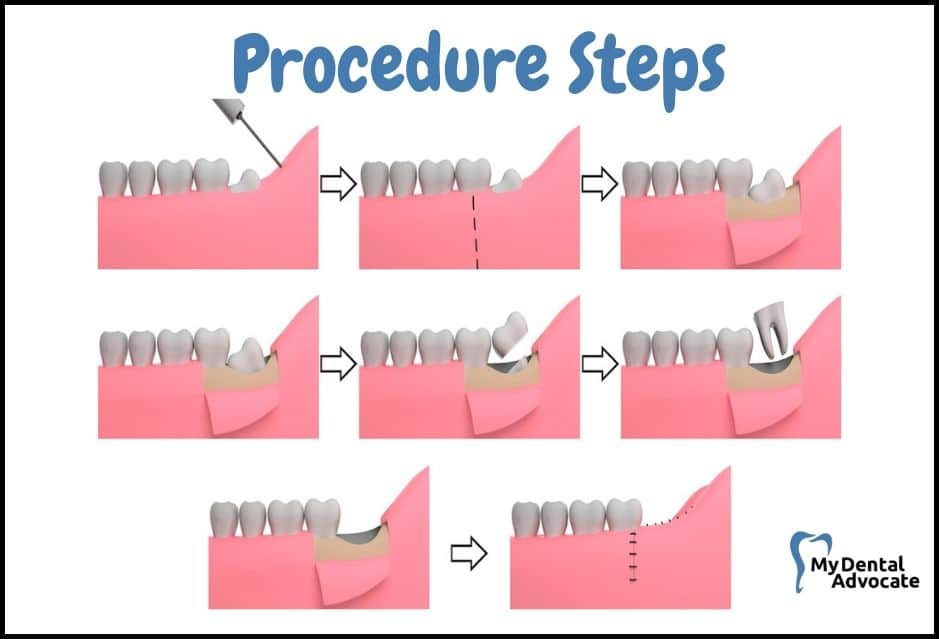
Procedure Steps
- Anesthesia/Sedation: The oral surgeon or anesthesiologist administers general anesthesia, making you “sleep” without recalling the procedure. Your vitals like blood pressure and heart rate are monitored.
- Local Anesthesia: This numbs your teeth area. Dental assistants will support your head and neck during the procedure.
- Incision: A cut is made behind the second molars for access to the wisdom teeth and bone.
- Bone Removal: Surgical tools remove bone around the tooth, carefully avoiding nerves and vital structures.
- Tooth Sectioning: The wisdom tooth is split into pieces for easier removal in the tight space.
- Extraction: The tooth is gently rocked and removed.
- Cleaning the Socket: The area is rinsed with sterile saline to clear any debris.
- Stitches: Sutures are placed to help form a blood clot and protect the area. These dissolve in 3-5 days.
- Recovery from Anesthesia: Medication is given to reverse anesthesia. You’ll be sleepy, so rest is important.
- Gauze Packs: These are applied to aid blood clot formation and should be kept in place for 30-60 minutes.
What’s Involved AFTER Wisdom Teeth Extractions?
After the procedure, the dental team will discuss post-operative instructions with your driver before heading home. The local anesthesia will wear off soon after, so take OTC Ibupfron and Tylenol (400 mg IBU + 1000 mg Tylenol) unless the surgeon prescribes prescription pain medication.
Be sure your pharmacy fills the pain medication before your procedure so you can take the medication BEFORE the local anesthesia wears off.
You may experience swelling, oozing, and mild discomfort for a few days after the procedure. Use a cold pack and anti-inflammatory OTC medications to minimize swelling.
Also, you may have difficulties opening and closing your jaw as the muscles have been stretched during the procedure. In addition, expect bleeding and oozing to occur for up to 24 hours.
Recommended Reading: How to Sleep After Wisdom Teeth Removal? (BEST Tips)Your surgeon will provide you with more detailed instructions, including changing the gauze if bleeding persists, avoiding physical activities for 3-5 days, and sticking with a soft-food diet for two weeks. Wisdom teeth extractions take two weeks to heal; however, call your doctor with any questions or concerns.
If antibiotics are prescribed and you are taking birth control pills, consider alternative birth control methods as birth control pills may be ineffective.
What to Eat After Wisdom Teeth Removal
Adequate nutrition after wisdom teeth surgery is essential to replenish your body with nutrients, vitamins and minerals to aid recovery. Your body spent many calories during the surgery and will continue spending calories for the next 1-2 weeks during the healing process.
Recommended Reading: What to Eat After Wisdom Teeth Removal? (BEST & WORST Foods)Dairy products such as yogurt, ice cream or milkshakes are not recommended soon after surgery, as nausea and vomiting may develop in conjunction with the anesthetic and pain medication.
Stick to foods such as mac & cheese, applesauce, scrambled eggs, soups, oatmeal and mashed potatoes. In addition, protein drinks provide a great source of nutrients in an easy-to-consume liquid formula.
Recommended Reading: 101 Foods to Eat After Dental Surgery, Implants or Wisdom Teeth RemovalCommon Complications After Wisdom Tooth Removal
Although every effort is made to minimize complications, 4.3% to 9.1% of cases result in some degree of complications.
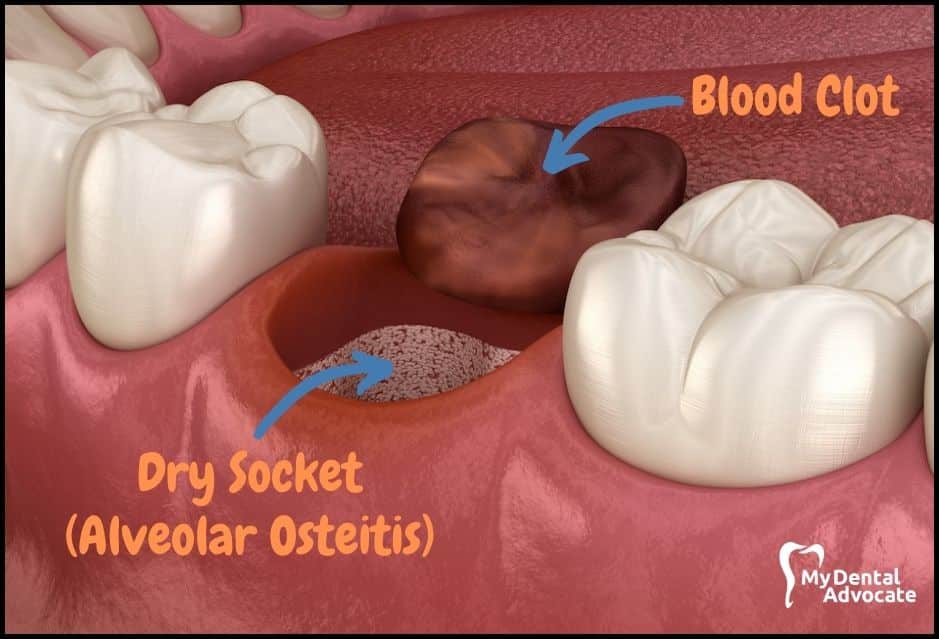
According to a recent study, the most frequent complication was alveolar osteitis (dry socket), occurring in 3.9% of cases. The second most common complication in 1.5% of cases was a post-operative temporary or permanent sensation disorder.
Managing post-operative complications becomes more challenging if immediate care is not taken.
When in doubt, call your dentist if you have any questions or concerns.
Managing Surgical Complications
- Dry Socket (Alveolar Osteitis): A common issue where the blood clot dislodges, exposing the bone and causing severe pain, usually around days 3-4. Treatment involves applying a special paste or irrigating with saline to form a new clot.
- Numbness (Paresthesia): This can happen if the inferior alveolar nerve near lower wisdom teeth is damaged. Studies show this occurs in 0.35% to 8.4% of cases. Though rare, it’s an important consideration for patients and dentists.
- Excessive Bleeding: Normal for up to 24 hours post-surgery, but if it continues, contact your dentist. Those on blood thinners may face this issue. Bite on a tea bag for temporary relief.
- Damage to Adjacent Teeth: Force used during surgery might inadvertently harm nearby teeth, like crowns or fillings. Most such damages are quickly fixable by your dentist.
- TMJ Issues: Surgery might stretch the TMJ, leading to temporary clicking or popping. If there’s no pain, it’s usually not a concern.
- Jaw Muscle Strain: The jaw muscles are stretched during the procedure, causing soreness or stiffness for 1-2 weeks. Use cold compresses initially, then alternate with warm packs. Limited jaw opening post-surgery is common.
- Swelling & Infection: Swelling and bruising are typical, but signs of infection like fever need immediate attention. Use over-the-counter anti-inflammatories for pain and inflammation.
- Nutrition and Recovery: Stay hydrated and eat a soft diet rich in carbs, protein, and vitamins (like mac & cheese, applesauce, protein shakes). Proper nutrition and sleep are crucial for healing.
Complete recovery of inferior alveolar nerve injury (IANI) occurs 6 to 8 weeks after the trauma, although it may take up to 24 months.
A dry socket occurs when the blood clot fails to form or falls out of the socket.
As a result, the exposed bone becomes inflamed and causes severe pain, predominantly in the lower extraction sites. Dry sockets commonly occur around day 3 or 4 and are highly unlikely to occur after one week.
According to the literature, the dry socket pain can last 7-14 days after surgery and the total healing time is increased.
Preventing Dry Socket
- Avoid using a straw, spitting or swishing vigorously up to 48 hours after surgery
- Allow warm salt water to pour out of your mouth when rinsing
- Avoid smoking & chewing tobacco up to 48 hours after surgery
- Avoid brushing the extraction site for 3-4 days
- Avoid crunchy, hot and spicy foods
- Consume a soft-food diet for 1-2 weeks after surgery
What Does a Dry Socket Look Like?
Dry sockets appear red, pink, or white. The red and pink coloration is the blood clot remnants left behind.
The white coloration is the infected bone surface that triggers the pain response. The tooth socket will be visible with minimal or no active bleeding.
Although there is a dry socket paste available (eugenol + cloves) that provides immediate relief, most clinicians will avoid applying it to the socket because it delays healing time and increases the chances of infection.
An alternative treatment method includes rinsing the tooth socket with sterile saline and curating (scraping) the socket walls to stimulate a new blood clot.
Increased Risk of Post-operative Complications
According to literature, post-operative complications are rare; however, they do occur. Many factors increase your chances of complications, including medical conditions, age, immune response and oral health.
Key Factors
- Diabetes
- Heart Disease
- Immunocompromised (HIV/AIDS, Cancer)
- Blood thinners
- Certain medications
- Poor oral health
- Poor surgical technique
- Incompetent surgeon
Is Top or Bottom Wisdom Teeth Removal Worse?
Generally, upper wisdom teeth are less challenging to remove because they are easier to access, and the upper jaw bone is thinner than the lower jaw bone.
In addition, the oral surgeon can remove the upper teeth without worrying about invading any major nerves or blood vessels in the area.
Lower wisdom teeth are more challenging to remove because the lower jaw bone is thick cortical bone, and impacted wisdom teeth can face many directions.
In addition, the oral surgeon has to be extremely careful not to damage the lower nerve (inferior alveolar nerve) as that may cause permanent lip numbness (paresthesia).
Oral surgeons are some of the most skilled and respected dentists because of their surgical expertise and technical abilities. Periodontists are also trained to remove wisdom teeth; however, they primarily focus on managing periodontal disease and placing implants.
Recovery After Wisdom Teeth Removal
Wisdom teeth removal is a standard outpatient procedure for patients between the ages of 15 and 25.
Recovery after wisdom teeth removal takes 3-4 days, but it can take 1-2 weeks for symptoms to subside. Your oral surgeon will provide detailed post-op instructions, including contact information.
In addition, you must follow the at-home care instructions that your surgeon gives you to prevent complications and to improve healing.
Your mouth is designed for optimal healing and regeneration; however, expect the tooth socket to take 3-6 months to heal completely.
Recommendations
- Take prescribed medication before the local anesthesia wears off
- Rest and recover for the first 3-4 days to allow the mouth to heal
- Avoid sucking, spitting, smoking or vigorously swishing to prevent dry socket.
- Use cold compress up to 36 hours after surgery to reduce inflammation, pain and swelling
- Alternate between hot and cold packs after that to stimulate healing
- Gently rinse mouth out with warm salt water 2-3x/day
- Gently massage TMJ and jaw muscles to decrease soreness
- Keep head elevated up to 72 hours after surgery to minimize pain and swelling
- Sleep often and stay off of your feet
- Avoid physical activity for 3-4 days
- Consume adequate amounts of fluid and electrolytes (Gatorade)
- Consume sufficient amounts of nutrients (soft-food diet)
Can You Work After Wisdom Teeth Removal?
Talk to your surgeon about their recommendations to return to work; however, most clinicians will encourage you to take 2-4 days off work after surgery.
Consider having your wisdom teeth removed over a holiday break, weekend or when you have time off of work to allow your body to rest and recover.
If you return to work, avoid physical activity or exertion, including bending, lifting or straining, as this will increase blood pressure, disturb the developing blood clot, and delay healing.
My Experience & Expertise
Wisdom teeth removal is a standard procedure to help you maintain oral health and minimize complications.
By understanding what’s involved in the surgery, including the recovery process, you’ll be better prepared for your surgery and know what to expect. If you have any questions or concerns, speak with your dentist.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!

What Are CEREC Crowns? (Advantages & Disadvantages)
With CEREC technology, dentists can create crowns in-office in just minutes. This guide will explain CEREC crowns, how they work, and what patients can expect from the same-day crown process…
Impacted Wisdom Teeth (How to Manage Symptoms)
Are you suffering from impacted wisdom teeth? If yes, then you should read this article. This condition is quite common and affects millions of people worldwide. Around 90% of us have at least one impacted wisdom tooth…

Philips Sonicare 9000 vs. 9300 Electric Toothbrush Review 2024
As a dentist with years of experience advocating for optimal oral health, I understand that the tools you use at home can make a significant impact on your dental well-being. Electric toothbrushes have become increasingly popular due to their efficacy and ease of use. But how do you choose the right one? Two standout models in my practice that have garnered attention are the Philips Sonicare 9000 and 9300 Electric Toothbrush.
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!