Endodontist (Root Canal Specialist)

When you refer to medical doctors, you know that includes doctors whose specialties range from pediatrics to orthopedics.
The same is true for dental doctors. Endodontists specialize in root canal therapy and related nerve tissue procedures.
Let’s look at other reasons why an endodontist would be beneficial to completing your next root canal.
Understanding Root Canals
Every tooth has a delicate inner pulp chamber that houses nerves and blood vessels to support sustainability and growth.
If trauma or bacteria disturbs this fragile area, an infection can arise, eliminating essential nutrients for the tooth. In addition, endodontists are skilled at providing adequate anesthesia, minimizing anxiety, and completing treatment promptly.
Endodontist accreditation requires 2-3 years of advanced education and training upon completing four years of dental school.
General dentists are trained to perform root canals; however, many refer to an endodontist. One of the reasons is that endodontists are trained to use chairside microscopes.
Recommended Reading:Five Qualities of a Great DentistAn endodontist can magnify the tooth up to 25x the original size, allowing exceptional visualization.
Endodontist Benefits
- Advanced training and education
- Microscope magnification used during treatment
- Unique tools to navigate curved roots
- Conscious sedation is possible
- Faster treatment compared to a general dentist
- Expert anesthetic administration
- Focused practice around root canals
Common Procedures
An endodontist’s most common procedures are initial endodontic therapy, endodontic retreatment, and apicoectomies.
Root canal therapy requires complete removal of the affected nerve tissue, bacterial debridement, and gutta-percha application.
However, they may be prone to re-infection if bacteria penetrate the inner chamber and progress into the roots.
The bacteria will proliferate and exit the end of the root leading to infection and possible abscess. If this occurs, the old root canal may need to be removed, debrided, and retreated.
The last technique is an apicoectomy, which removes the infection at the root base, bypassing the existing root canal. The disease is accessed through the gum and bone tissue along the side of the jaw.
Initial Endodontic Therapy
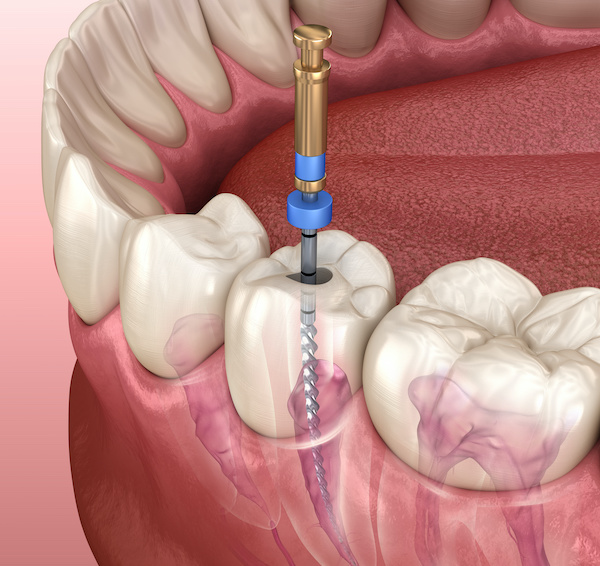
As we’ve discussed before, if bacteria have entered the nerve space, also known as the pulp chamber, removal is necessary to eliminate the bacteria and prevent future microbial invasion.
After an adequate anesthetic is administered, the assistant will place a rubber tent around the planned tooth to limit contamination and avoid irrigation solution entering the mouth.
Next, the clinician will enter the nerve space and remove the nerve.
You should be adequately numb; however, immediately let your clinician know if you feel any pain.
The clinician will then enter each root and remove the remaining nerve tissue, carefully navigating the twist and turns.
Then, mechanical and chemical antibacterial irrigants will be applied to the roots to verify adequate debridement.
After this, the dentist will use gutta-percha material into each root to seal off bacteria and prevent microbial re-infection. You may wonder how the clinician knows where to stop at the end of the root.
They use a specialized file machine to calculate and measure each root in millimeters.
Root canals can be tedious and technique sensitive, so it’s best to have an endodontist perform this procedure when in doubt.
After completion, a temporary filling will be placed, and the clinician will advise you to return to your general dentist for crown fabrication.
Although rare, let’s look closely at the most common reasons root canals fail.
Root Canal Failure
- Bacterial contamination during the procedure
- Infected nerve tissue left in roots
- Contamination while waiting for the final crown
- Lack of completion of the final crown
- Underfilled root canal/poor technique
- Cavity forms under the crown, leading to re-infection
- Bacterial leakage around temporary filling
- Fractured instrument in the root
- Missed root canal during treatment
Your endodontist will be focused on limiting these points of failure. Root canal therapy has been around for many years and has stood the test of time for safety and efficacy.
Approximately 15 million root canals are performed each year in the U.S. alone.
Endodontic Retreatment
The leading cause of root canal failure is bacterial persistence within the root canal or coronal leakage after the completion of the final restoration.
Therefore, weighing the pros and cons of root canal retreatment versus extraction is essential.
The literature reports a success rate ranging from 80-88% for endodontic retreatment.
However, many factors are considered. These factors include clinical expertise, minimal root curvature, adequate isolation, diagnosis, and therapeutic success.
General dentists are rarely trained to perform root canal re-treatments, so it’s advised to have an endodontist perform it.
After adequate anesthesia and isolation, the previous crown is carefully removed. At this point, the clinician will better understand if the root canal failed because of decay or bacteria persistence within the root canal.
Removing the previous root canal requires time.
Next, the clinician will remove the remaining bacteria using mechanical and chemical means, then re-apply gutta-percha.
Finally, they’ll place a temporary filling and send you back to your general dentist. There are scenarios where the endodontist can access the root canal through the old crown if a root canal is advised for reasons other than decay under the crown.
If this occurs, a permanent filling will be used to seal off bacteria after treatment completion.
Apicoectomy
If an endodontist sees an infection on the x-ray and the root canal appears acceptable, they may consider an apicoectomy, which requires drilling through the side of the jaw at the level of the root tip.
The endodontist must accurately predict where the root tip is located compared to the gingival margin and adjacent teeth.
After accessing the root tip beneath the bone, the clinician will remove the bacteria and debride the area to remove the source of the infection.
Material is then applied to seal the root canal and prevent bacteria contamination. Sometimes bone graft material is placed around the root if a bony defect is present. Sutures will be used to encourage proper healing.
Related: Learn more about Dental ImplantsAccording to reports, there’s a 90% success rate for apicoectomies due to advances in technology and techniques.
Considerations
Initial root canal therapy has a high 85-95% success rate and allows patients to preserve their natural tooth rather than have it extracted.
If extraction is desired, a dental implant is the most common method for replacing teeth. This procedure is considered the “gold standard” for replacing teeth.
Other options include a removable partial denture if multiple teeth need to be replaced. The last option is a permanent bridge that secures the adjacent teeth. Before committing to any treatment, discuss what option is best for you with your provider.
Related: Best MDA Recommended Products
My Experience & Expertise
Root canal therapy is an effective procedure that can relieve pain and heal a damaged tooth.
Have you recently been diagnosed with needing a root canal? Are you aware of the alternative options?
My Dental Advocate’s team of board-certified dentists can provide a second opinion on your planned treatment. We look forward to bringing you peace of mind by verifying your treatment plan, suggesting an alternative, or answering your questions.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!

Can You Reverse a Cavity? (5 Simple Steps)
Cavities that are located in the enamel can be reversed. This process is called remineralization and can only be accomplished when the cavity is superficial. If the cavity progresses to the dentin layer…
Does Fluoride During Pregnancy Affect Child’s IQ?
As a dentist, I’m often asked about the safety and effectiveness of fluoride use during pregnancy. Recent research has explored the potential link between fluoride exposure during pregnancy and its effect on a child’s IQ…
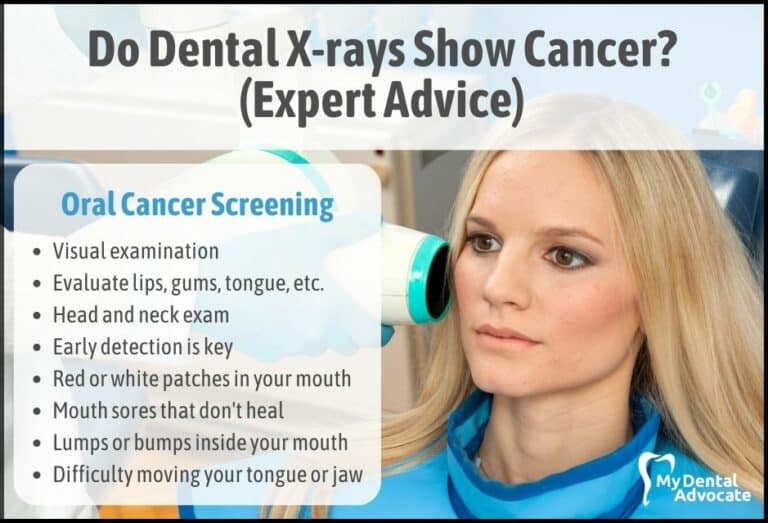
Do Dental X-rays Show Cancer? (Expert Advice)
When we step into a dental office for a routine checkup, one of the common procedures we encounter is the dental X-ray. Often, these X-rays are taken to help dentists identify hidden dental abnormalities, cavities, or gum disease.
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!