Oral Surgeon (Procedures & Considerations)

Oral surgeons are essential dental community members as they’re also the last line of defense when treating dental disease, pathology, or malformations.
Oral surgeons’ scope of practice encompasses multiple procedures and settings.
Extractions, including wisdom teeth, and dental implants, are the most commonly performed procedures.
Recommended Reading: Wisdom Teeth Removal Cost 2024 (With & Without Insurance)Understanding Oral Surgeons
Oral Surgeons preform many procedures as mentioned, along with performing biopsies, treating TMJ, managing myofascial pain, exposing impacted teeth for orthodontic-assisted eruption and diagnosing oral pathology.
Oral surgeons also have hospital privileges to perform reconstruction and cosmetic surgery, treat maxillofacial trauma, correct cleft and craniofacial deformities, correct maxillofacial deformities, and perform orthognathic surgery.
After completing dental school, oral surgery accreditation requires 4-6 years of further education and training.
Clinical Practice Procedures
The most common procedures in a clinical setting are extractions, including wisdom teeth, and placing implants.
They routinely use conscious, deep, or general anesthesia for pain and anxiety control. Most oral surgeons have their practice; however, some will travel to the general dentist’s office for satellite care.
They’re equipped with essential equipment and supplies to perform procedures, including sedation. Pathology biopsies are not routinely performed when satellite care is provided, as patient follow-up is difficult.
Wisdom Teeth Extractions
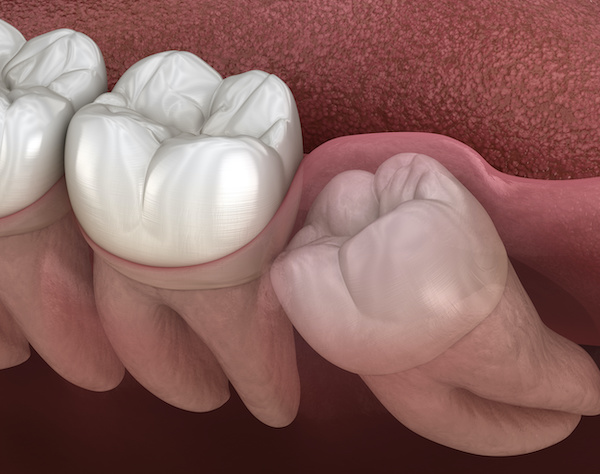
Wisdom teeth, also known as third molars, are commonly removed due to limited space in the mouth.
Impacted teeth can lead to infection if the tooth partially erupts and bacteria enter below. If there’s enough space in the mouth, wisdom teeth will begin to erupt around 18 years of age.
If the tooth is ideally positioned and has an unobstructed path to erupt, it will erupt as planned if adequate space is present.
Although an ideal eruption may occur, many patients will have challenges keeping these teeth clean because of their location in the mouth, often leading to decay and infection.
It’s recommended to have your wisdom teeth removed between the ages of 15 and 25 to prevent this and prevent forward pressure on the remaining teeth.
Wisdom teeth extractions are a standard procedure performed under anesthesia.
It will take 30-60 mins and best be completed early in the morning as fasting will be required 8 hours prior.
It’s recommended to have this procedure performed over a school break or time off, as recovery will take 1-2 weeks.
Most patients require removal because their wisdom teeth are impacted and growing in the desired direction.
If surgery is performed after 25, patients may have more challenges recovering because the roots will be further embedded deep in the bone.
The inferior alveolar nerve (IAN) runs adjacent to the wisdom teeth, so the surgeon will evaluate the position of the nerve before the procedure.
Most of the time, the IAN is a safe distance away from the tooth; however, occasionally, the roots can wrap around the nerve leaving tooth removal impossible. In this case, the surgeon will leave a portion of the root not to damage the nerve during removal.
In addition, your provider will administer general or IV sedation during the procedure to aid in pain and anxiolytic relief.
IV Sedation
- High level of sedation
- Effects are felt quickly
- Shorter recovery time
- Produces temporary amnesia
- Reduces gag reflex
- Patient remains conscious
General Anesthesia
- Highest level of sedation
- Used when tolerance is high
- Best for impacted wisdom teeth
- Unable to respond or feel pain
- Produces amnesia
- Gag reflex is eliminated
Recommended Reading:
- Wisdom Teeth | The Ultimate Guide (Content Hub)
- Wisdom Teeth Removal (What’s Involved?)
- Impacted Wisdom Teeth: Symptoms, Causes, Removal & Recovery
- What to Eat After Wisdom Teeth Removal? (BEST & WORST Foods)
- 101 Foods to Eat After Dental Surgery, Implants or Wisdom Teeth Removal
- Wisdom Teeth Removal Cost 2024 (With & Without Insurance)
- How to Sleep After Wisdom Teeth Removal? (BEST Tips)
- Sedation Options for Wisdom Teeth Removal (Read this FIRST)
- Wisdom Tooth Pain: Symptoms, Relief & Home Remedies (Helpful Tips)
- 10 SIMPLE Steps to Prepare for Wisdom Teeth Surgery
Postoperative Instructions
If sedation is being performed, the patient will need someone to drive them home after the appointment.
Patients will be encouraged to bite on gauze for 30-60 mins to promote blood clot formation. The dentist will likely provide pain medication and antibiotics to prevent infection.
It’s essential to begin taking pain medication before the anesthetic wears off. Be cautious when eating, avoiding biting cheeks and lips.
Soft food diet is recommended for 1-2 weeks, depending on extraction severity and recovery. Avoid smoking, spitting, sucking, or anything that could dislodge the blood clot and lead to a dry socket.
The dentist may provide an antibacterial rinse (Chlorhexidine) to aid in food removal and limit bacteria growth.
Lightly brush around extraction sites to prevent food buildup from occurring. Patients may have difficulties opening and closing their jaw for a few weeks until the muscles have recovered.
After two weeks, contact your provider for follow-up care if pain, infection, or swelling is still present.
Dental Implants
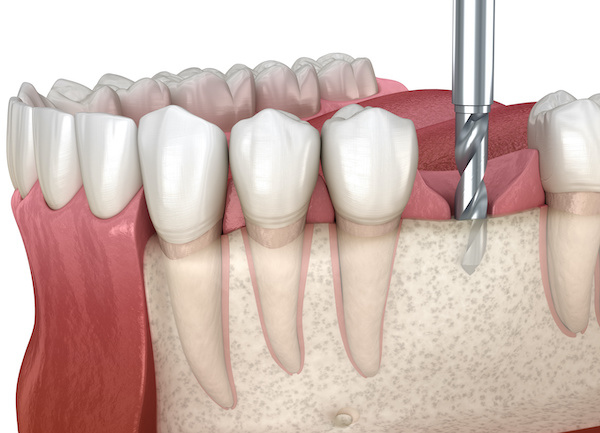
Implants have become increasingly popular over the past 20 years because of technological advances, research, and development.
Implants are the best option to replace missing teeth as they best resemble natural teeth.
However, many implant systems exist, so it’s essential to document the brand and specifications to provide your general dentist with accurate crown fabrication.
Also, in the future, if a problem arises and you need to replace the crown, the clinician will need the information to order the correct parts for accurate fitting.
Implants are classified as immediate or delayed depending on their placement stage. For example, if the implant is placed on the same day as tooth removal, it’s considered an immediate implant.
On the other hand, an implant will be placed four months after the extraction if extraction is performed and a bone graft is placed for healing.
Learn more about the pros and cons of the two implant techniques.
If an immediate implant is placed, the surgeon will also place a bone graft and secure the site with a resorbable membrane to encourage osseointegration.
After four months, the surgeon will confirm that integration has occurred by torquing the implant to a specific degree.
If stability and health are ensured, the general dentist will take an impression, fabricate the crown, and secure it to the implant body. Strict protocols are in place for each implant system regarding torque specifications.
If a delayed implant is planned, the implant will be placed four months after the extraction.
Key Considerations
Oral surgeons are trained to manage oral pain and ease anxiety. They’re equipped with skills and techniques to navigate these challenges.
Many oral surgeons desire a consult before any procedure to verify the medical history and answer any questions or concerns.
They also specialize in extracting multiple teeth before denture placement. It’s not uncommon for patients to have full-mouth extractions during a single visit.
Oral surgeons are exceptional at managing dental disease; they’re also skilled at handling complex health issues.
They are greatly valued for treating medically compromised patients or too challenging for a general dentist.
Related: Best MDA Recommended ProductsMy Experience & Expertise
Oral surgeons are highly-trained specialists in the dental community.
Most patients will need their services between 15 and 25 years of age. Have you recently been diagnosed with needing extractions or dental implants? Are you concerned about your planned treatment?
My Dental Advocate’s team of board-certified dentists can provide a second opinion on your planned treatment. We look forward to bringing you peace of mind by verifying your treatment plan, suggesting an alternative, or answering your questions.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!
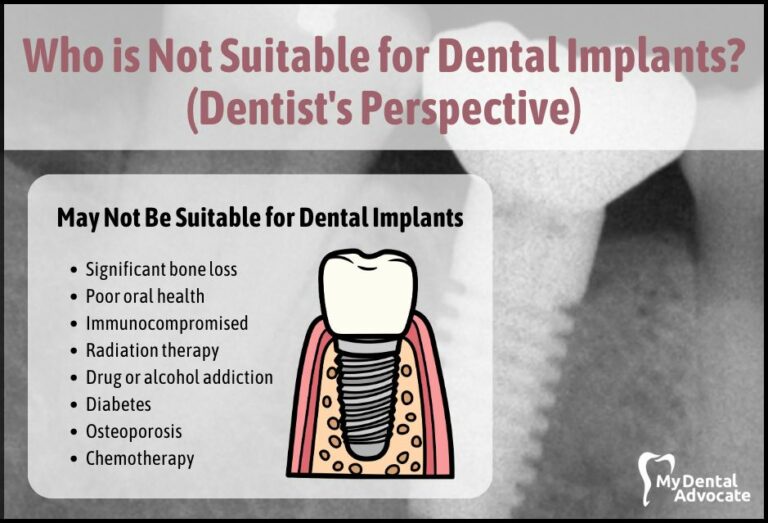
Who Is Not Suitable for Dental Implants? (Dentist’s Perspective)
Dental implants are a popular and effective way to replace missing teeth. They are a permanent solution that can improve oral health and restore your smile. However, not everyone is a good candidate for dental implants…
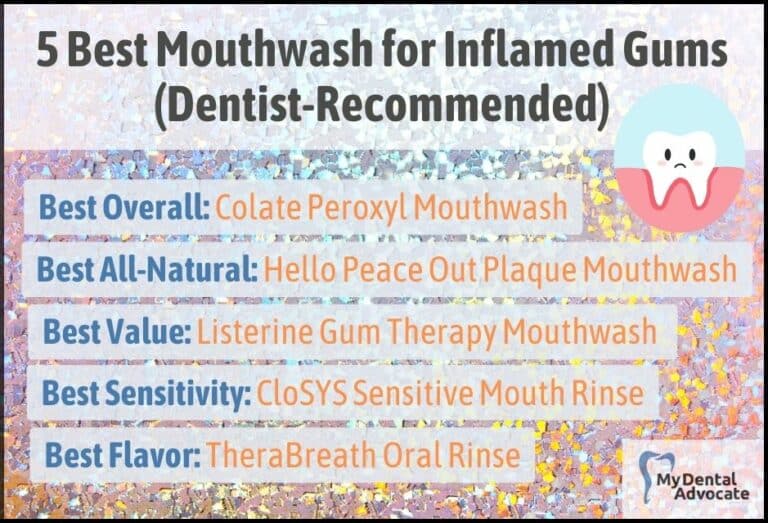
5 Best Mouthwash for Inflamed Gums 2024 (Dentist Recommended)
Gum inflammation can be a real nuisance. It causes discomfort and sensitivity and can lead to more serious oral health issues if left untreated. If you’ve ever experienced that sore, swollen feeling in your gums, you know the importance of relief and prevention.
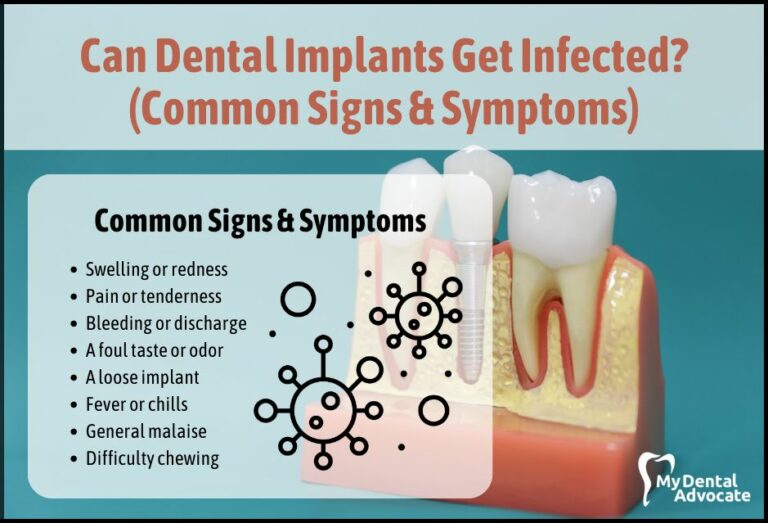
Can Dental Implants Get Infected? (Common Signs & Symptoms)
Imagine stepping out with a brand new, confident smile thanks to your dental implants. But wait, did you know even these cutting-edge solutions can sometimes face an unexpected challenge – infections?
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!