What Is Scaling & Root Planing?
Heart disease is one of the most common diseases affecting 48% of adults.
But did you know there’s another disease nearly as prevalent and could indicate heart health?
Researchers are still working to identify a link, but gum disease could be a risk factor for heart disease.
The good news is that the dentist or dental hygienist can treat gum disease early and effectively.
It starts with scaling and root planing.
What Is Periodontal Disease?
Periodontal disease, or periodontitis or gum disease, is a severe infection affecting the gums and bone supporting the teeth. It’s caused by bacteria that have accumulated deep below your gum line.
According to a recent Centers for Disease Control and Prevention (CDC) report, 47% of adults 30 years and older have periodontal disease. The prevalence increases with age, as 70% of adults 65 years and older have periodontal disease.
Recommended Reading: 5 Best Mouthwash for Receding Gums 2024 (Dentist Recommended)What Is Scaling and Root Planing?
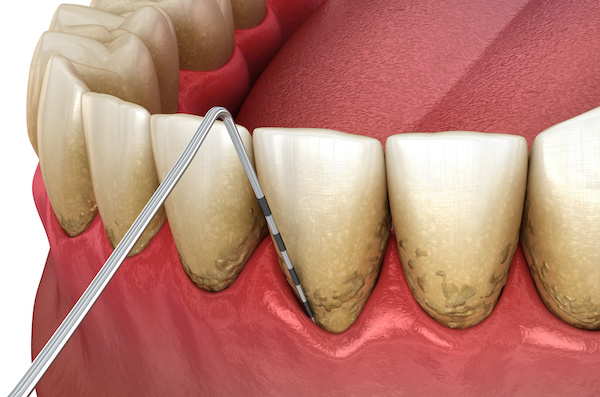
Scaling and root planing (SRP), also known as deep cleaning, removes bacteria above and below the gum line when inflammation and bone loss are present, known as periodontitis.
As we discussed in the prophylaxis section, bacteria thrive in difficult areas to clean.
Below the gumline is home to the most aggressive bacteria in your mouth. They embed deep into the gum tissue and adhere to the root surface if they’re not removed.
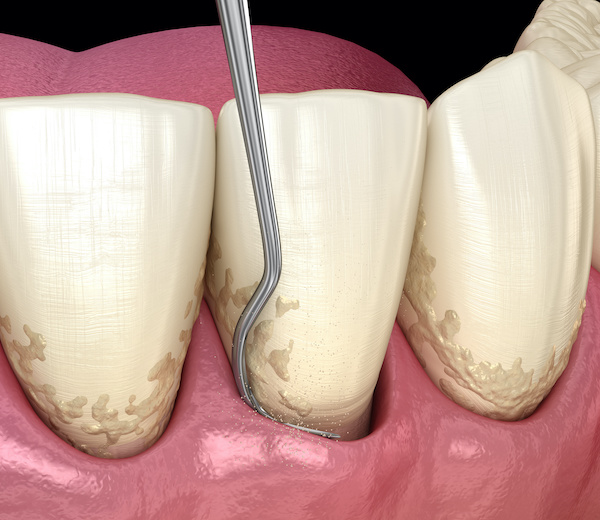
Initially, they assemble into a sticky solution known as plaque, and over time they form “rock-like” crystals known as calculus or tartar. Bacteria become extremely difficult to remove, similar to a barnacle on the back of a seashell.
Scaling and root planing treatment is the only way to remove bacteria below the gum line.
What are Periodontal Probings?
The periodontal probe is essential to assess and evaluate the gum attachment level within the sulcus, where the teeth and gum tissue meet. Your clinician or dental hygienist will record measurements within the gingival sulcus at six different sites.
Probe Measurements
- 1-3mm Measurements: Indicates healthy gum attachment, with shallow pockets easy to clean through brushing, flossing, or Waterpik use.
- 4mm Measurements: Suggests potential failure of gum attachment due to bacteria irritating the gums.
- 5-7mm Measurements: Shows compromised attachment, with bacteria nearing the bone, causing bone loss and making non-surgical cleaning harder.
- 8+ mm Measurements: Indicates advanced gum disease, requiring a Periodontist’s intervention for surgical cleaning to control bacteria and prevent tooth loss.
Your hygienist will most likely be measuring your gums.
However, don’t be alarmed if your dentist chooses to record the measurements. Healthy gums don’t bleed, so if you taste blood after the probing is complete, you may have areas of inflammation, also known as gingivitis.
Fortunately, this is reversible, so work with your clinician to improve home care before gum disease progresses.
How Is Periodontal Disease Diagnosed?
After recording gum measurements, your clinician will evaluate your x-rays, analyzing the bone level around your teeth. If bone loss is noted, the dentist will diagnose periodontal disease.
The measurements confirm if the disease process is currently active or stable.
An “active stage” means bacteria thrive subgingivally, causing severe inflammation, infection, and bone loss. Scaling and root planing will be diagnosed and is the first step to restoring your gums.
However, if bone loss is present and your gum measurements are between 1 and 4 mm, your periodontal disease is most likely stable. Don’t let your guard down, as you’re still at risk for active periodontitis in the future.
What Happens During Treatment?
As discussed earlier, scaling and root planing involves cleaning the bacteria deep below the gum line. Unfortunately, this process is uncomfortable for most individuals.
There are multiple ways to achieve pain relief. Cetacaine is a needle-free topical solution applied within the gingival sulcus to prevent pain at the source.
If more pain relief is needed, a local anesthetic can be administered.
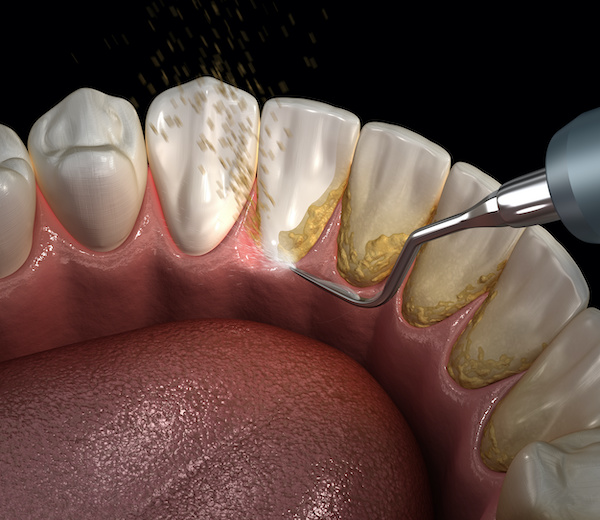
After adequately numbing the gums, your hygienist will use various hand instruments and an ultrasonic scaler to remove the tenacious calculus deep below the gum line.
Don’t be alarmed if your gums bleed during this process; this is common.
Your hygienist will complete half the mouth during the first visit and the other half at a future visit. Then, if time allows and you’re tolerating the procedure well, full mouth scaling can be completed.
Lastly, the teeth are polished and flossed, and fluoride is applied if desired.
Common Adjunctive Procedures
Periodontal disease can be challenging to manage, and sometimes we have to throw the kitchen sink at it. We’re mechanically removing the bacteria during the scaling and root planing process; however, there are ways to fight the bacteria chemically.
Adjunctive Procedures
- Diode Laser: Combined with scaling and root planing, it kills bacteria by heating tissue below the gum line around the tooth.
- 2% Chlorhexidine Gluconate: An antiseptic used in dental offices, applied via ultrasonic scaler or syringe, effectively attacking bacteria.
- Arestin: An antibiotic for deep pockets, works over several days. Post-application, avoid flossing the area for ten days to let it reduce pocket depth, especially effective in 6+ mm pockets.
Postoperative Instructions
Your clinician may inform you to avoid eating hot or spicy foods for the remainder of the day. Also, your teeth and gums may be sore and tender, so protect them from being damaged inadvertently.
Brushing and flossing after is well tolerated and encouraged to maintain gingival health.
Periodontal disease is always present, so it’s essential to have routine periodontal maintenance to prevent re-infection. Periodontal maintenance will be recommended every 3 to 4 months, depending on your home care, medical history, and gum disease severity.
If the dentist or dental hygienist cannot control the gum disease, further surgical intervention will be needed with a Periodontist.
Related: Best MDA Recommended ProductsMy Experience & Expertise
Periodontal disease is prevalent in our population today.
However, it’s commonly underdiagnosed, which is unfortunate because, in addition to possible links with heart disease, the bacteria that cause gum disease are also associated with the development of Alzheimer’s disease and dementia.
Have you recently been diagnosed with gum disease? Are you comfortable with your treatment plan? My Dental Advocate’s team of board-certified dentists can provide a second opinion on your planned treatment.
We look forward to bringing you peace of mind by verifying your treatment plan, suggesting an alternative, or answering your questions.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!

Best Dental Advice (Dentist Perspective) | Part 1
According to a recent study, Only 25.8% of children reported a high oral health knowledge. Yet, we have many resources to learn about healthy dental habits, revolutionary dental products, and preferred dental treatments…

10 BEST Steps to Prepare for Wisdom Teeth Surgery 2024
So you scheduled an appointment to have your wisdom teeth removed. Now what? How do I prepare for wisdom teeth removal? What’s involved? Feelings of anxiety are expected before the day of surgery…

Bitvae D2 Ultrasonic Electric Toothbrush Review 2024
Let’s face it, brushing your teeth isn’t the most exciting part of your day. But what if I told you there’s a toothbrush that can make your oral care routine effective and enjoyable? Enter the Bitvae D2 Electric Toothbrush, a dental tool…
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!