Can You Reverse a Cavity? (5 Simple Steps)
Did you know you can heal cavities without dental treatment?
According to the Centers for Disease Control and Prevention (CDC), 90% of adults have had a cavity, and 1 in 4 adults currently have a cavity.
Cavities can be a real pain, and nobody enjoys paying money to have their teeth drilled on.
Healing a cavity can save you money, time, and unnecessary pain, but you may need your dentist’s help.
Need Dental Advice? Ask Dr. Hannan!
Can You Reverse a Cavity?
Cavities that are located in the enamel can be reversed.
This process is called remineralization and can only be accomplished when the cavity is superficial. If the cavity progresses to the dentin layer, the cavity cannot be repaired because there’s an irreversible hole in the tooth. There are five simple steps to heal a cavity.
Related: Learn more about Cavities
How Do Cavities Form?
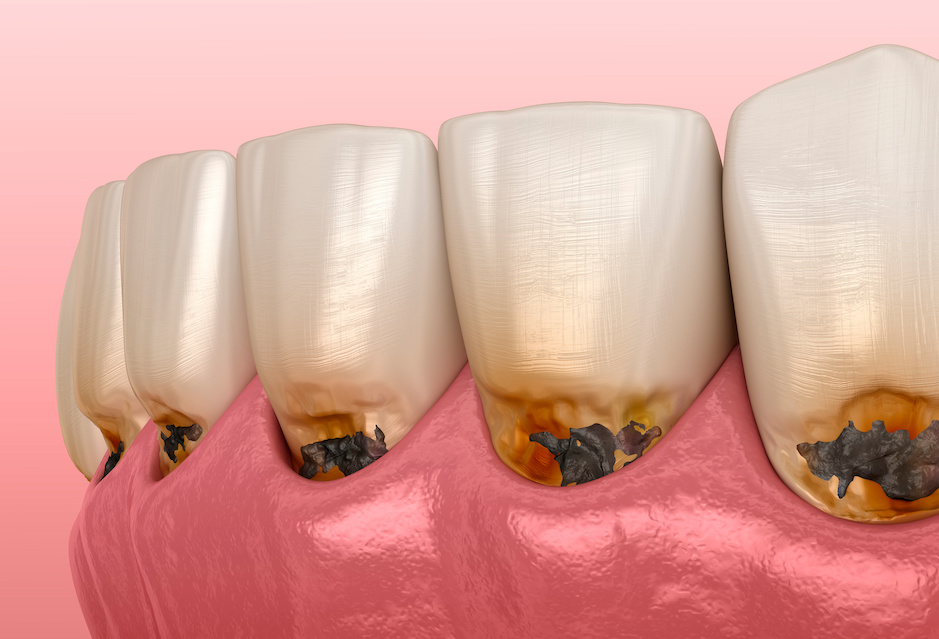
Cavities, also called tooth decay or caries, are holes in teeth that require enamel repair or dental treatment.
Tooth decay occurs when bacteria in your mouth consume sugars from the food you eat to produce acid and damage the tooth surface. Many factors contribute to tooth decay, summarized in the image below.
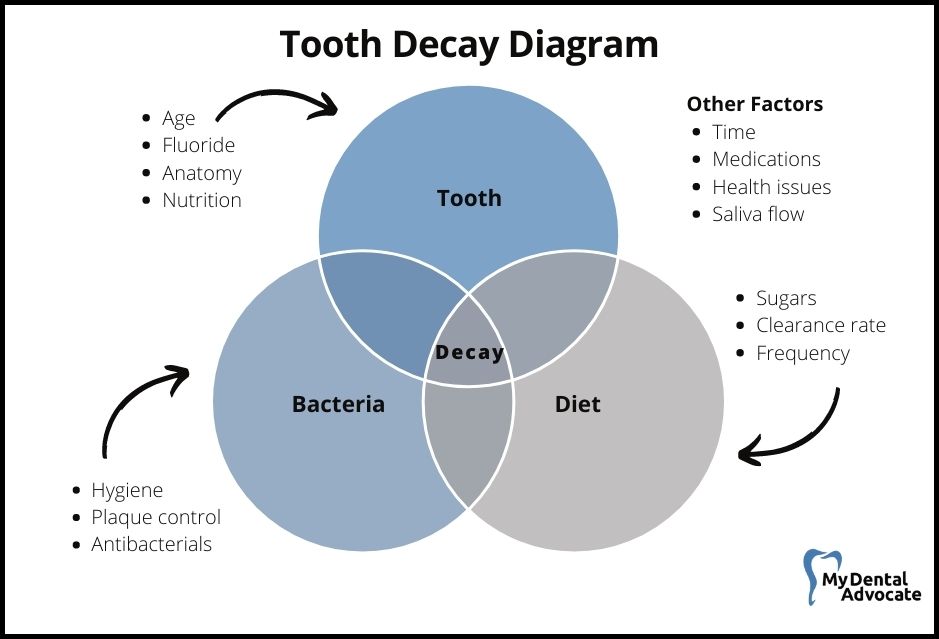
Tooth Decay Risk Factors
Everyone with teeth is at risk for tooth decay.
However, some individuals have an increased cavity risk because of many factors.
Cavities are one of the greatest unmet health treatment needs and, if left untreated, can lead to problems eating, speaking, playing, and learning.
Key Factors
- Tooth Location: Back teeth, especially molars and premolars, are harder to clean and more prone to decay due to their grooves and pits.
- Poor Oral Hygiene: Inadequate brushing and flossing increase plaque and bacteria, leading to tooth decay. Plaque should be removed promptly.
- Dry Mouth: A dry mouth environment promotes cavity formation. This condition can result from certain medications or low saliva production.
- Poor Nutrition: High-sugar diets feed cavity-causing bacteria. Lack of water consumption also impedes the clearing of food particles, increasing decay risk.
- Poor-Fitting Restorations: Gaps in crowns and fillings create spaces for bacteria, leading to a higher chance of tooth decay.
- Infrequent Dental Visits: Regular dental check-ups and cleanings are crucial to identify early signs of decay and remove plaque and calculus.
- Genetics and Medical Issues: Some people are naturally more susceptible to cavities due to weaker enamel or a tendency to harbor bacteria. Certain medical conditions can also weaken the immune system, affecting the body’s ability to combat bacteria.
Recommended Reading: 12 Cavity Risk Factors (Best Treatment)
Common Signs & Symptoms
The size and severity of the cavity correlate to how deep it penetrates the tooth.
The tooth is made of three layers enamel, dentin, and pulp, and the deeper the hole, the more painful it becomes. Cavities progress at varying stages depending on the location and other risk factors.
Occasionally cavities are present, and the patient is unaware due to the absence of pain.
Signs & Symptoms
- Spontaneous pain (Toothache)
- Pain from stimulation (sweet, hot, or cold)
- Pain when biting down
- Visible holes in teeth
- Black, brown, or white stains on teeth
When to Visit the Dentist
Regular dental visits and cleanings are essential to prevent tooth decay.
Most cavities form in hard-to-reach areas without pain or irritation. The dentist is trained to recognize early signs and symptoms to repair weakened enamel. If pain is present, visit your dentist for evaluation and treatment.
Recommended Reading: 10 Simple Steps to Prevent Cavities (Dentist’s Perspective)
Cavity Management & Treatment
Dentists will formulate a treatment plan based on your medical history, x-rays, and exam.
Smooth surface cavities in the enamel layer are the simplest to repair with topical fluoride application. The fluoride adheres with the weakened enamel to form a new solid bond.
Cavities that advance past the enamel require more advanced dental treatment.
Common Dental Treatments
Recommended Reading: Colgate Hum Electric Toothbrush Review5 Simple Steps to Heal a Cavity
These five steps provide the most significant opportunity to reverse a cavity and are listed from most important to least important.
Cavities only localized in the first tooth layer (enamel) can be healed/remineralized.
Tooth decay that advances into the second tooth layer (Dentin) or further requires dental treatment because an irreversible hole in the tooth needs repair.
Step 1: Nightly Fluoride Trays (Dentist Required)
Nightly fluoride trays are fabricated at the dentist and require an upper and lower impression of your teeth.
Your dentist will also prescribe 1.1% sodium fluoride anti-cavity gel to apply inside the trays.
When you wear them each night, fluoride will be in direct contact with your teeth to remineralize cavities.
Step 2: Prescription Fluoride Toothpaste (Dentist Required)
Your dentist can also prescribe 1.1% sodium fluoride anti-cavity toothpaste that you should use nightly.
Use a pea-sized amount, and after thoroughly brushing, spit it out and don’t rinse.
Rinsing your mouth will inadvertently remove the fluoride minerals and prevent tooth remineralization.
Step 3: Topical Fluoride Varnish (Dentist Required)
5% fluoride varnish is only available at your dentist and can be directly applied to localized areas of decay.
The sticky varnish is gently painted on your teeth and requires no eating or drinking for at least 30 minutes.
The direct application provides a protective barrier for fluoride to take effect.
Step 4: Over-the-Counter Toothpaste
The most effective remineralizing toothpaste contains sodium fluoride, stannous fluoride, or calcium phosphate (hydroxyapatite).
These ingredients bond to weakened enamel, repairing missing tooth structures and preventing future decay.
Look for one with the American Dental Association (ADA) Seal of Acceptance.
Recommended Reading: What is the ADA Seal of Acceptance?Step 5: Oral Health Improvement
Oral health improvement consists of regular dental visits, frequent brushing, and nightly flossing.
Antibacterial mouthwash also helps remove food particles while killing cavity-causing bacteria. However, improving oral health may require mastering new dental.
Recommended Reading: Top 10 Habits for Improved Oral HealthMy Experience & Expertise
Cavities that are located in the enamel can be reversed and healed.
The advances in fluoride use and treatment have been impactful.
Fluoridation of drinking water and other fluoride cavity-prevention treatments is a top 10 public health achievement in the 20th century. Visit your dentist regularly to screen for tooth decay and prevent future dental problems.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!
Sources
- “Cavities”. Centers for Disease Control and Prevention (CDC)
- “Cavities/Tooth Decay”. Mayo Clinic
- American Dental Association (ADA)

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!

Does Matcha Stain Teeth? The Truth About Matcha and Teeth Stains
Matcha is a trendy superfood that’s become a staple in many people’s diets. But for some, the thought of drinking matcha may be met with concern about teeth staining. In this article, we’ll uncover the truth about matcha and teeth stains…
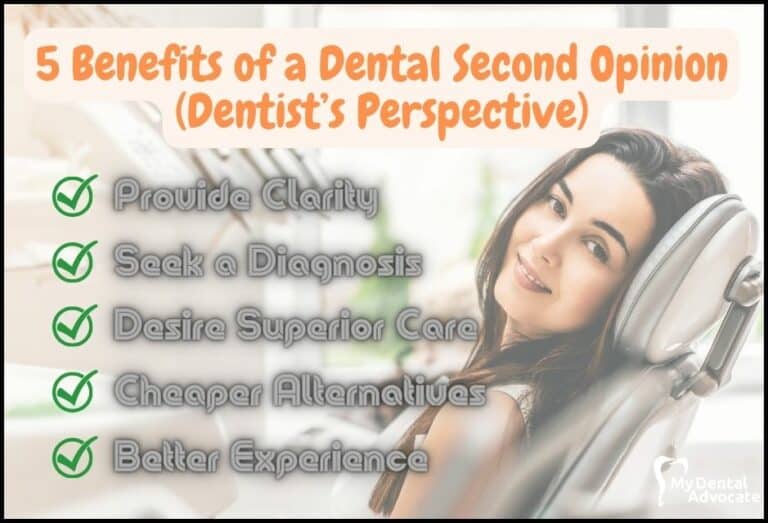
5 Benefits of a Dental Second Opinion (Dentist’s Perspective)
Visiting a dentist is stressful enough. If you’re diagnosed with hundreds or thousands of dollars of dental work, your stress goes thru the roof. So do you take the dentist’s word or seek a second opinion? What are the benefits of a second opinion? Second opinions provide clarity for proposed dental treatment…
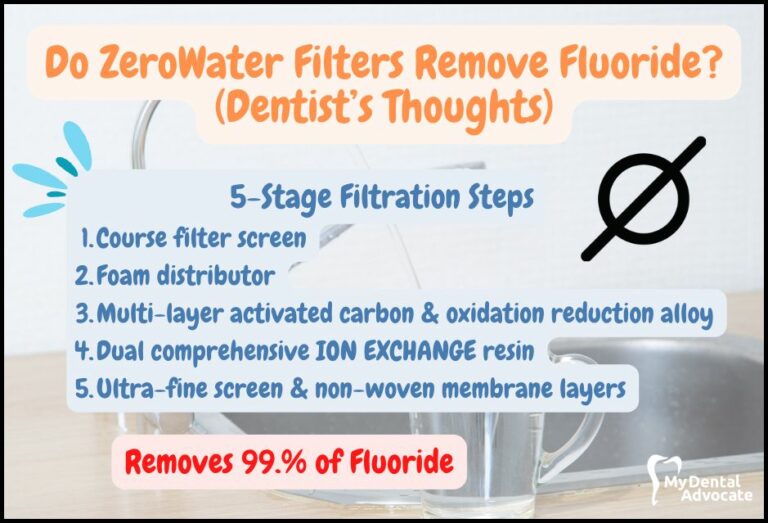
Do ZeroWater Filters Remove Fluoride?
Water filtration systems have become a popular choice for many households looking to improve the quality of their drinking water. ZeroWater and Brita are two of the most well-known brands in the market, with millions of users worldwide. While Brita uses a basic filtration system, ZeroWater…
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!