Acute Necrotizing Ulcerative Gingivitis (ANUG) “Trench Mouth”
Although I’ve never treated a patient with acute necrotizing ulcerative gingivitis (ANUG), I can only imagine the pungent odor that would be evident.
As a dentist, I know the smell of periodontal disease. It’s a distinct odor that occurs when bacteria have localized deep below the gums and infect bone and gum tissue.
Acute necrotizing ulcerative gingivitis is a rare form of gum disease. However, understanding this oral condition may encourage improving your oral health.
Recommended Reading: Gingivitis | The Ultimate GuideNeed Dental Advice? Ask Dr. Hannan!
What Is Acute Necrotizing Ulcerative Gingivitis (ANUG)?
Acute necrotizing ulcerative gingivitis (ANUG) is a rare infectious disease of the gums, affecting <1% of the population.
This oral disease most commonly occurs in an impaired host immune response.
For example, a patient undergoing cancer treatment or immunocompromised is more susceptible to ANUG because their body has a limited ability to fight off harmful bacteria and infection.
ANUG is a severely destructive form of gum disease that’s characterized by distinct signs and symptoms.
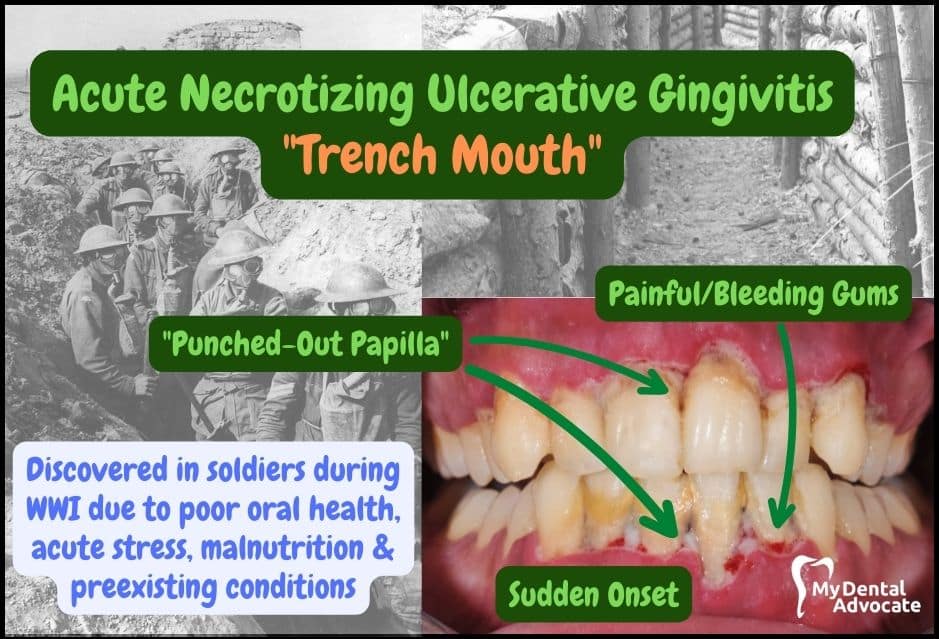
Signs & Symptoms
- Punched-out papilla
- Sudden onset of inflammation
- Painful, bleeding gums
- Crater-like gum lesions
- Halitosis
- Lymphadenopathy
- Malaise
Acute necrotizing ulcerative gingivitis (ANUG) presents as gram-negative bacteria known as spirochetes.
Why Is It Called “Trench Mouth”?
Acute necrotizing ulcerative gingivitis (ANUG) is commonly referred to as “trench mouth” because of its occurrence among soldiers in the trenches during World War I.
It’s closely associated with stress and anxiety experienced by soldiers during the war.
Today, ANUG readily presents in adolescents and teenagers during acute stress if they have other conditions, including hormonal changes, poor oral hygiene, and immunocompromised.
Recommended Reading: What is Gingivitis? Causes, Symptoms & Treatment
ANUG is also commonly associated with smoking because it drys the mouth and alters the bacterial flora. Harmful oral bacteria, including cavity-causing bacteria, thrive in dry, acidic environments.
In addition, trench mouth can be prevalent in individuals with poor oral health and hygiene.
Best Oral Care Routine
- Brushing (use an electric toothbrush)
- Flossing (or water flosser)
- Use mouthwash nightly
- Regular dental checkups (every six months)
- Routine cleanings
- Avoid sticky sweets
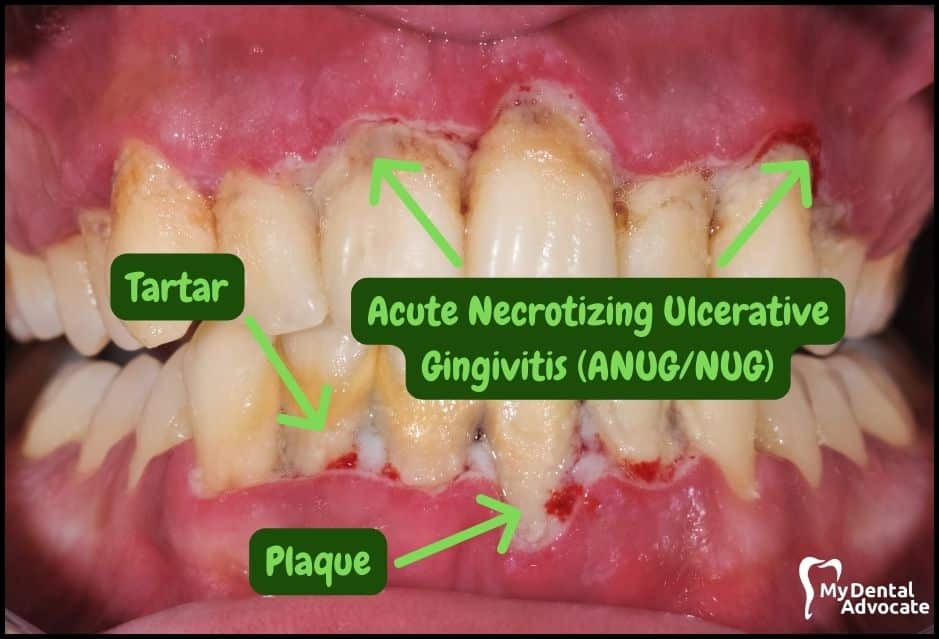
What Is Necrotizing Ulcerative Gingivitis (NUG)?
Necrotizing ulcerative gingivitis (NUG) is a distinct and specific form of periodontal disease without the acute (sudden) onset.
It has been given many names: Vincent’s disease, fusospirochetal gingivitis, trench mouth, acute ulcerative gingivitis, necrotizing gingivitis, and acute NUG.
Recommended Reading: Gingivitis vs Periodontitis (Gum Disease) | Dentist’s PerspectiveThe diagnosis of NUG follows three clinical features, including papilla necrosis, bleeding, and pain.
In addition and similar to ANUG, the identification of risk factors that alter the host response leads to increased risk. In addition, treatment should be purposeful, well-organized and detailed across multiple dental providers.
The most crucial step during treatment is immediately addressing the acute phase to prevent sequelae (further harm) and craters in soft tissues.
What Causes “Trench Mouth”?
Trench mouth is related to many predisposing factors, including acute stress, immunosuppression, malnutrition and poor oral hygiene.
These conditions, along with the formation of dental plaque, result in the overgrowth of bacteria in the interdental area leading to “punched-out papilla.” Invasion of the bacteria into the tissue causes NUG.
The exact causative organisms have not been identified; however, most ANUG and NUG patients involve the following microorganisms.
Common Organisms
- Prevotellaintermedia
- Fusobacterium species
- Treponemaspecies- T. vincentii and T. buccalis
- Selenomonas species
Diagnosis Characteristics
Understanding acute necrotizing ulcerative gingivitis (ANUG) and the most common clinical factors will prevent a patient from being misdiagnosed.
For example, ANUG is commonly confused with other bacterial and viral conditions.
Bacterial & Viral Conditions
- Gonococcal or streptococcal gingivitis
- Acute herpetic gingivostomatitis
- Infectious mononucleosis
- Desquamative gingivitis
- Multiforme erythema
- Pemphigus vulgaris
Best Treatment
Prompt and timely treatment of ANUG is paramount to the overall treatment success. Therefore, the treatment of ANUG should be addressed in three successive stages.
Treatment of Acute Phase
The primary goal of the acute phase treatment is to halt tissue destruction and control the patient’s discomfort.
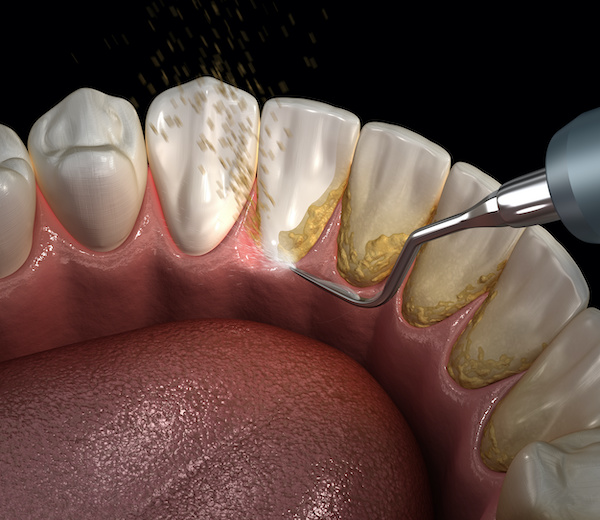
For example, the dentist gently removes superficial gingival plaque and calculus with an ultrasonic scaler. Local anesthetic or other topical numbing agents may be needed for patient comfort.
In addition, 0.12% Chlorhexidine Gluconate, an oral antibacterial rinse, will be used to irrigate in and around the gum tissue to eradicate harmful bacteria chemically.
Systemic antibiotics such as Metronidazole (250 mg 3 x daily) will be considered.
Antibiotic Treatments
- Penicillin
- Tetracyclines
- Clindamycin
- Amoxicillin
- Amoxicillin + Clavulanate
According to a recent study, oral penicillin invoked significant clinical improvement after 3-6 days.
Treatment of Preexisting Conditions
After the acute phase has been controlled, treatment of any preexisting conditions, such as chronic gingivitis, should be initiated.
In addition, this stage involves professional prophylaxis (cleaning) in the form of scaling and root planning and establishing oral hygiene home-care habits that the patient can use daily.
Predisposing factors will also be addressed, including smoking, poor sleep habits, poor oral hygiene, and acute stress.
In addition, The dentist or dental specialist can perform a gingivectomy procedure to treat gum damage and prevent disease progression.
Treatment of Disease Sequelae & Maintenance
The main goal of the maintenance phase is to comply with the best oral hygiene practices and control any predisposing factors. If proper maintenance is not carried out, relapses are likely to occur.
The treatment of ANUG consists of a multifactorial approach between various dental providers.
Prognosis
Prompt diagnosis and treatment will prevent irreversible damage to the underlying bone and gum tissue.
In addition, comprehensive treatment prevents the progression of the disease.
Nevertheless, according to a recent study, a lack of treatment can lead to gum deterioration—potentially fatal conditions include necrotizing ulcerative periodontitis (NUP) and even cancrum oris (noma).
If ANUG is left untreated, improperly treated or neglected, it will become chronic and recurrent.

Common Factors
- Psychological stress
- Poor diet
- Insufficient sleep
- Alcohol & tobacco use
- Poor oral hygiene
- Preexisting gingivitis
- HIV infection
Should I Be Concerned?
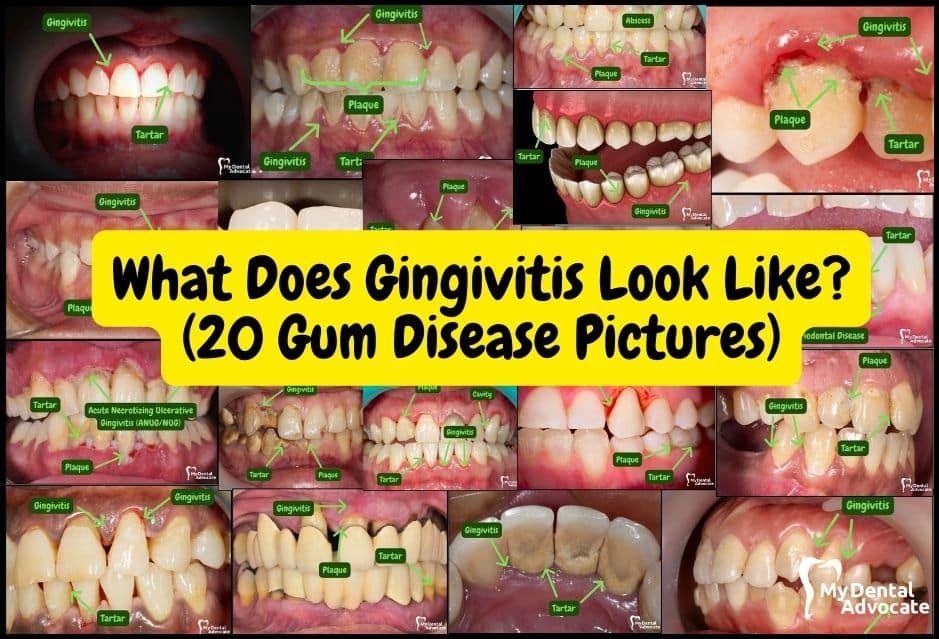
Healthy gums are vital to a patient’s oral and systemic health.
Maintaining excellent oral hygiene is the most effective way to avoid developing gingivitis and other severe gum diseases.
Studies show that the harmful bacteria that cause gum disease can lead to significant health issues, including Alzheimer’s and cardiovascular disease.
Health conditions like HIV infection, diabetes, and cancer can reduce a person’s ability to fight infection, increasing the risk of developing gum disease.
Although acute necrotizing ulcerative gingivitis (ANUG) is rare, certain factors correlate with increased likelihood.
For example, anti-seizure medications, some blood pressure medications, hormonal changes, and tobacco use can heighten your risk.
However, keeping gums healthy and preventing oral gum disease is possible with daily care and regular visits to a dentist.
My Experience & Expertise
Acute necrotizing ulcerative gingivitis (ANUG) and other severe gum diseases pose a diagnostic dilemma to clinicians.
Diagnosing and coordinating treatment with an interprofessional team approach can be challenging.
Though there are specific diagnostic criteria to diagnose ANUG, patients may exhibit non-specific signs and symptoms or only meet some of the diagnostic criteria.
Regardless of the particular presentation, recognizing the potential and likelihood of necrotizing gum disease is critical and will prevent irreversible damage.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!

BURST Teeth Whitening Trays Review (Dentist Recommended)
BURST teeth whitening trays are their newest product that features fast-acting results after one 15-minute session. In addition, after completing the 7-day course, you’ll notice dramatically whiter teeth. Say goodbye to the nasty chemical taste…

Best Dentist-Recommended Gum (Top Picks)
Chewing gum has long been a popular pastime, but not all gums are created equal regarding oral health. Some can even offer dental benefits when chosen wisely. Dive into our list of the top 5 dentist-recommended gum that not only freshen your breath but also promote a healthier mouth.
Dental Second Opinion | The Ultimate Guide (Content Hub)
Dental second opinions are essential for expert oral health care, clarity and peace of mind. Are you considering a second opinion? My Dental Advocate can help! Read this ultimate guide to learn more…
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!