Understanding Gingivitis: Causes, Symptoms & Effective Treatments
Have you recently visited the dentist for a basic cleaning only to hear you have gingivitis?
You’re not alone; 94% of Americans have gingivitis.
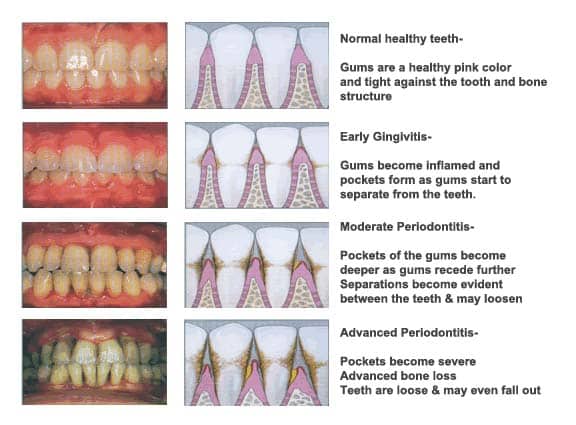
If gingivitis is left untreated, it can progress into gum disease, also known as periodontal disease.
Periodontal disease consists of irreversible bone loss that can lead to loose teeth. Understanding gingivitis causes, symptoms and treatment options will help eliminate harmful bacteria for improved oral health.
Need Dental Advice? Ask Dr. Hannan!
What Is Gingivitis?
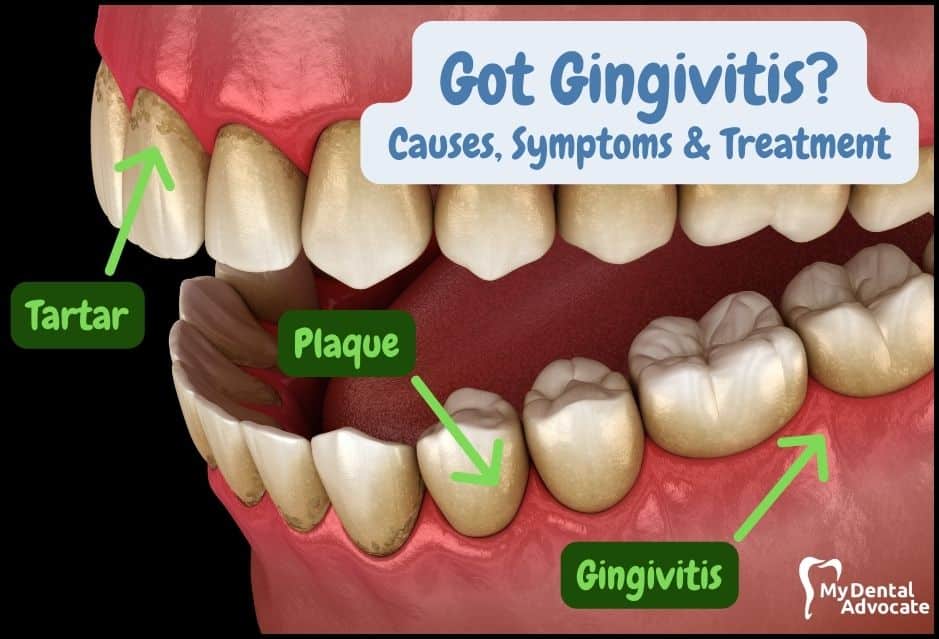
Gingivitis is inflammation of the gums caused by harmful bacteria.
If your dentist or hygienist does not remove harmful bacteria, the bacteria will congregate and multiply into advanced gum disease (periodontal disease).
The bacteria that infects the gums lead to swollen, red and puffy gums. Gingivitis is a common gum issue; however, oral hygiene improvements can help prevent this ailment. According to the American Dental Association, gingivitis and periodontitis cause tooth loss in adults.
Common Causes
- Why Good Oral Hygiene Matters: Not brushing and flossing leads to dental plaque and gum inflammation. Regular dental visits and good hygiene can remove this plaque. If ignored, it can turn into severe gum disease.
- The Role of Nutrition: Harmful bacteria love sugars and carbs. They grow when you eat these foods. Brushing, flossing, and dental cleanings stop these bacteria from harming your gums. Sticky, sugary foods are especially bad for oral health.
- What is Dental Plaque? It’s the fuzzy feeling you get on your teeth when food debris isn’t cleaned off. Plaque bacteria feed on sugars, creating acids that inflame your gums. Brush twice a day and floss every night to control plaque.
- Tartar and Its Impact: If plaque stays on your teeth, it turns into tartar under the gumline. Tartar attracts more bacteria and shields them. It also irritates and inflames gums. Unlike plaque, you can’t remove tartar at home – it requires a professional dental cleaning.
Signs & Symptoms
It’s possible to have gingivitis without any symptoms.
However, in mild cases of gingivitis, there may be no discomfort or noticeable symptoms. Often, it remains undetected for quite some time. The symptoms of gingivitis are somewhat non-specific.
Additionally, the pink-salmon coloring and stippling in the gum tissue will often disappear. Also, the gums may appear shiny as the gum tissue becomes inflamed and stretched over the tissue surface.
Common Signs
- Red & purple gums
- Swollen & puffy gums
- Gum inflammation & discoloration
- Gum separation & recession
- Bleeding gums
- Halitosis (bad breath)
Common Symptoms
- Tender gums
- Pain when chewing
- Sensitive teeth & gums

When the gums are swollen, the lining becomes ulcerated, and the gums are prone to bleed even with gentle brushing and flossing.
In addition, if the gums are inflamed, they may start pulling away from the neck of the tooth.
This causes gaps between the teeth and the gums, known as gum pockets (or periodontal pockets).
Recommended Reading: What Does Gingivitis Look Like? (20 Gum Disease Pictures)Similarly, many people aren’t aware that they have gum disease (periodontal disease). Periodontal disease, also known as periodontitis, can cause teeth to shift position, wobble or hurt when you chew. In addition, periodontal disease will lead to irreversible bone loss.
Periodontal disease is treated with scaling and root planing, also known as deep cleaning. If gum disease is not controlled, your dentist will refer you to a gum specialist known as a periodontist.
Common Risk Factors
Specific risk factors increase the likelihood of developing gingivitis and periodontitis. Certain medications, such as antiseizure and immunosuppressants, can lead to gingival hyperplasia (gum overgrowth).

Other Risk Factors
- Smoking or chewing tobacco
- Dry mouth
- Hormones
- Vitamin C deficiency
- Immunosuppressants
- Cardiovascular drugs
- Leukemia & HIV/AIDS
- Suppressed immunity
- Cancer
- Diabetes
- Pregnancy (hormones)
- Genetics (family history)
- Viral & fungal infections
- Orthodontics/braces
- Stress/anxiety
- Depression
- Crooked teeth
- Poor-fitting dental appliance
- Poor-fitting fillings
- Poor oral hygiene
Diagnosis
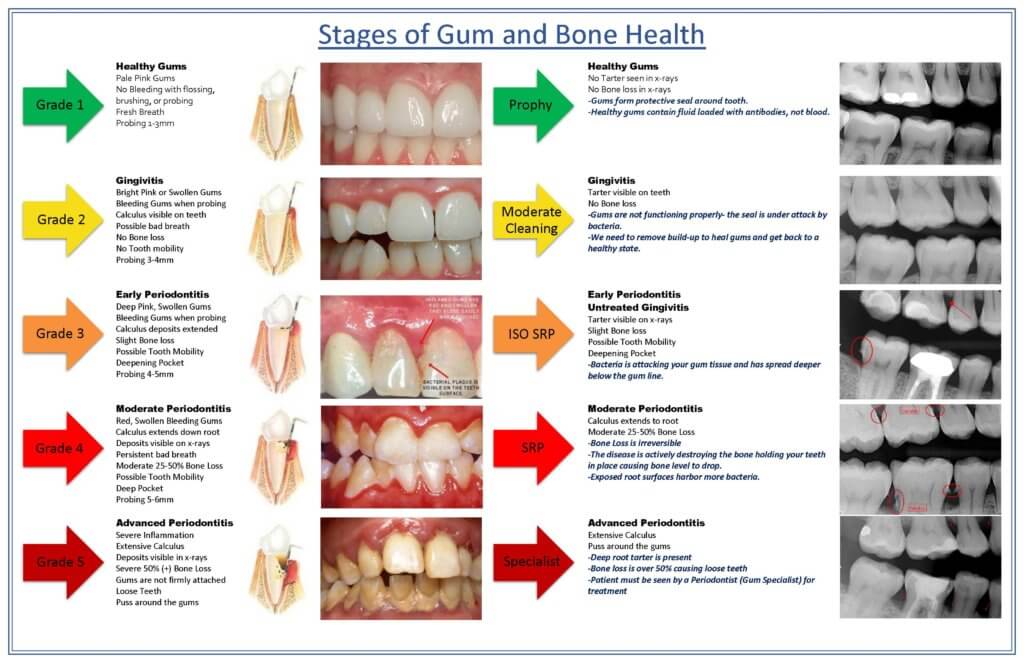
Your dental exam consists of an intraoral and extraoral exam along with complete series of dental x-rays. X-rays allow the dentist to check for cavities and bone loss.
In addition, the clinician will probe your gums with a dental instrument to check gum inflammation. The small millimeter measuring tool measures pockets around your teeth.
Typical gum measurement depths are 1 to 3 millimeters.
Recommended Reading: 14 Gingivitis Home Remedies That Work! (Dentist Recommended)A dentist or hygienist will check for gingivitis signs, including gum inflammation, plaque and tartar around your teeth. Gingivitis is a precursor to periodontal disease.
Periodontal disease is different than gingivitis in that there is gum inflammation + bone loss.
In addition, gingivitis is reversible, unlike periodontal disease, which is irreversible. Gum disease can be managed but is classified as either active or inactive. Periodontal maintenance cleanings work to maintain gum disease in an idle state.
Recommended Reading: Pregnancy Gingivitis: Causes, Symptoms & Treatment 2024Common Complications
Following the clinicians instructions will typically prevent further complications.
Chronic gingivitis is associated with systemic diseases such as respiratory disease, diabetes, coronary artery disease, stroke and rheumatoid arthritis.
In addition, research suggests that the bacteria responsible for periodontitis can enter your bloodstream through the gum tissue, possibly affecting your heart, lungs and other body parts.
Other Complications
- Periodontal Disease: A Serious Concern: If gingivitis isn’t treated, it can turn into periodontal disease, affecting the tissue and bone around teeth. This serious condition can lead to tooth loss.
- Trench Mouth: A Severe Gum Infection: Known medically as Acute Necrotizing Ulcerative Gingivitis (ANUG), trench mouth is a painful, severe gum disease with bleeding and ulcers. It’s rare in developed countries but more common where there’s poor nutrition and living conditions.
- Abscesses in Gums and Teeth: Bacteria from gingivitis and periodontal disease can infect the tooth root, causing an abscess. A periodontal abscess occurs in the gums, while a tooth abscess is at the tooth root.
- Recurrent Gingivitis: The Cycle of Inflammation: If bacteria above the gums are removed but left below, gingivitis can come back. Regular cleanings remove bacteria above the gums but can trap bacteria below, leading to repeated gingivitis.
Treatment (Evidence-Based Research)
The clinician will educate you about the disease if you are diagnosed with gingivitis or periodontitis.
In addition, they will review how to properly care for your mouth. Treatment for gingivitis includes cleaning the gums and teeth above and below the gum line.
Dental scaling instruments are used to remove plaque and tartar. In addition, an ultrasonic scaler rapidly vibrates to remove tenacious tartar.
I recommend having your dentist smooth any ledges or rough edges of fillings and crowns. These issues will snag floss and harbor harmful bacteria that can lead to gum disease and tooth decay.
Other treatment recommendations include:
In-Office Treatment
- Chlorhexidine for Gingivitis: Recent studies show chlorhexidine mouth rinse reduces gingivitis. It’s available for both in-office and at-home use (by prescription). But be aware, long-term use can stain teeth.
- Laser Therapy’s Benefits: Research indicates low-level laser therapy lessens gum inflammation. Combining laser therapy with chlorhexidine is even more effective for reducing gum inflammation. It’s a common treatment for periodontal disease.
- Fluoride Treatment’s Role: A study found that stannous fluoride (0.45%) effectively reduces gingival bleeding. The reduction is even greater when combined with a prophylaxis cleaning.
- Arestin for Deeper Issues: Arestin (Minocycline HCl) microspheres, used with scaling and root planing, can reduce pocket depths. This antibiotic targets bacteria below the gum line.
At-Home Treatment
- Electric Toothbrushes: A Smarter Clean: Electric toothbrushes outperform manual ones in removing plaque and bacteria. They come with timers, brushing detection, subscription brush heads, and oscillating technology.
- The Importance of Flossing: Flossing removes bacteria between teeth effectively. Use a “C-shaped” method for best results. Water flossing is great for cleaning larger gaps between teeth.
- Water Flossing and Gingivitis: Studies show using a water flosser with an antibiotic mouthwash can control gingivitis-causing bacteria.
- Hydrogen Peroxide for Gum Health: Research suggests short-term use of hydrogen peroxide can control gingivitis. Fluoridated hydrogen peroxide mouth rinses also help remove stains and reduce gingivitis.
- Antibacterial Mouthwash for Comprehensive Cleaning: Brushing reaches only 25% of your mouth. Listerine’s antibacterial mouthwash kills bacteria and plaque in 30 seconds. Mouthwashes with essential oils like thymol, menthol, and eucalyptol offer anti-inflammatory benefits.
Best Prevention
Gingivitis is a highly prevalent gum issue; however, you can prevent it.
If your family has gum disease, you may face a greater risk of developing it. In addition, you may need more frequent checkups and cleanings to prevent gum disease.
Recommended Reading: Is Gingivitis & Gum Disease Contagious? (What the Research Says)
Encourage your family members to have their teeth cleaned to avoid spreading harmful bacteria between members. Talk to your dentist and dental hygienist about specific recommendations.
Best Prevention Methods
- Use electric toothbrush
- Brush twice daily
- Floss regularly
- Use mouthwash
- Regular dental visits
- Don’t smoke or use tobacco
- Control diabetes (other medical issues)
- Eat balanced diet
Gingivitis vs. Healthy Gums
Gingivitis
- Bright pink gums
- Swollen gums
- Bleeding gums
- Plaque present
- Bad breath (possible)
- Probing 3-4 mm
- Tartar present
- No bone loss
Healthy Gums
- Pale pink gums
- No bleeding
- Fresh breath
- Probing 1-3 mm
- No tartar
- No bone loss
Gingivitis vs. Gum Disease (Periodontal Disease)
Gingivitis
- Bright pink gums
- Swollen gums
- Bleeding gums
- Plaque present
- Bad breath (possible)
- Probing 3-4 mm
- Tartar present
- No bone loss
Gum Disease
- Red or purple gums
- Swollen gums
- Bone loss
- Tooth mobility
- Bad breath
- Probing 4+ mm
- Tartar present
Frequently Asked Questions (FAQ)
My Experience & Expertise
The prevalence of gingivitis is exceptionally high.
If you’ve been diagnosed with gingivitis, don’t panic. Treat gingivitis by using an electric toothbrush twice daily, flossing nightly, visiting your dentist regularly and maintaining excellent oral hygiene.
If you don’t have gingivitis, well done. Review the prevention section to maintain health.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!
Dental Second Opinion | The Ultimate Guide (Content Hub)
Dental second opinions are essential for expert oral health care, clarity and peace of mind. Are you considering a second opinion? My Dental Advocate can help! Read this ultimate guide to learn more…
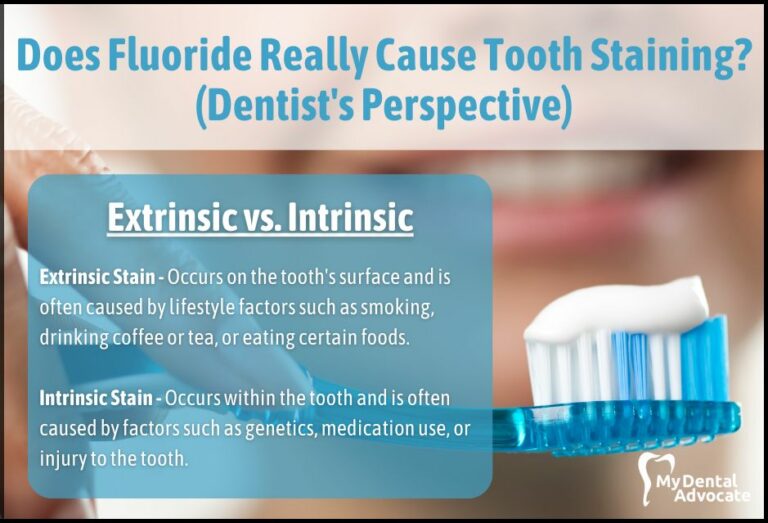
Does Fluoride Cause Tooth Staining? (Expert Advice)
Fluoride is a superhero in fighting tooth decay, but does it come with a catch? Some people worry that using fluoride can lead to unsightly tooth stains. In this post, we’ll explore the science behind fluoride and tooth staining…
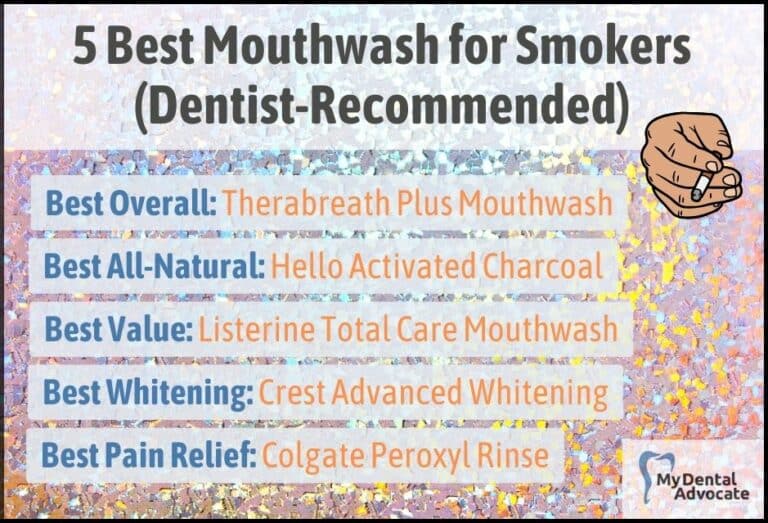
Best Mouthwash for Smokers (Dentist Recommended)
For smokers, regular oral care isn’t just about freshening breath; it’s about maintaining overall oral health. Combating the specific challenges tobacco poses, such as staining and bacteria buildup, requires a specialized regimen.
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!