Sleep After Wisdom Teeth Removal? (Dentist Advice)
According to a recent study, 73% of high school students don’t get enough sleep—unfortunately, the percentage skyrockets after wisdom teeth extractions.
Wisdom teeth removal is necessary for most 15 to 25-year-olds, and much of the planning and preparation revolves around the surgery.
Immediately after surgery, you are fatigued and need to rest; sleep is a top priority.
Recommended Reading: Wisdom Teeth | The Ultimate GuideNeed Dental Advice? Ask Dr. Hannan!
Wisdom Teeth Removal
Wisdom teeth or third molars are the last adult teeth to erupt and are located in the back of the mouth.
They come in between the ages of 15 and 25, and 85% of Americans will have them removed. Most people have four wisdom teeth (two on top and two on the bottom).
However, it’s possible to have one, two, three, or more than four; the extra teeth are called supernumerary teeth.

After wisdom teeth surgery, you may experience swelling, inflammation, and discomfort for a few days.
Expect bleeding and oozing to occur for up to 24 hours. Use a cold pack and anti-inflammatory OTC medications to minimize pain and swelling.
In addition, you may have difficulties opening and closing your jaw as the muscles have been stretched during the procedure.
The healing process after third molar extractions can be taxing.
Restful sleep is vital to minimize symptoms and decrease recovery time. Sleeping also promotes healing, repair and recovery.
For example, you will have more pain without restful sleep, and it will take longer for your mouth to heal. In addition, inadequate sleep can lead to anxiety, depression and mood swings.
Recommended Reading: Wisdom Teeth Removal Cost 2024 (With & Without Insurance)How to Sleep After Wisdom Teeth Removal
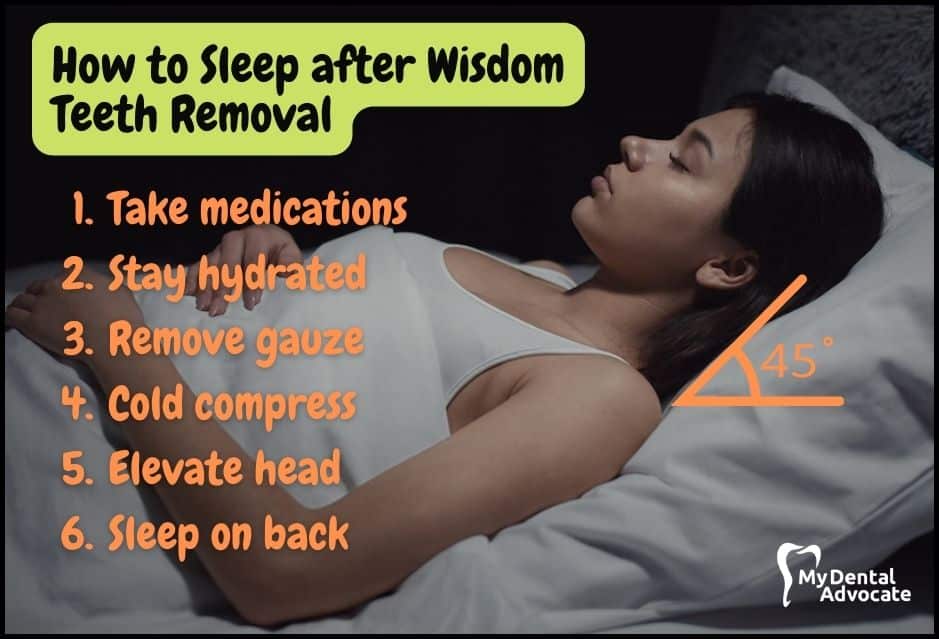
Sleeping modifications are necessary to minimize swelling, prevent dry socket and decrease pain.
For example, you should sleep on your back to avoid inadvertently damaging the healing tooth sockets. In addition, you should elevate your head above your heart at a 45-degree angle. This position allows sufficient blood to flow to and from the extraction site.
Let’s explore the best tips for a restful night’s sleep from a dentist’s perspective.
Recommendations
- Take Medications Promptly: After wisdom teeth removal, take pain medication as soon as possible. It’s best to have it ready before the procedure for immediate use when the numbness fades.
- Stay Hydrated for Faster Recovery: Drink plenty of water to help your body heal. Aim for 8 ounces of water 8 times a day. Proper hydration speeds up recovery and reduces pain.
- Gauze Management: Bite on gauze for 30-60 minutes post-surgery. If bleeding continues, keep using gauze until it stops. Remember to remove gauze before sleeping to avoid choking.
- Use Cold Compress: Applying a cold compress or ice pack reduces pain and swelling. It constricts blood vessels and muscles, lessening discomfort.
- Elevate Your Head: Keep your head higher than your heart for 24-36 hours to minimize swelling. Use pillows or sleep in a recliner to maintain a 45-degree angle.
- Sleep on Your Back: Avoid sleeping on your side to prevent pressure on your jaw. Back sleeping keeps your posture upright and protects the surgical area. Expect some bleeding, so protect your pillow with a towel or use an old pillowcase.
Additional Tips & Advice
Create a comfortable sleeping environment so you can calm your mind and optimize your chance of restful sleep.
Sleep research is one of the fastest-growing areas of study because so many people suffer from sleep loss.
According to the CDC, 1 in 3 Americans are sleep deprived and receive less than 7 hours of sleep. Yet, countless studies recommend 7-9 hours of sleep each night to repair your mind, increase energy and improve focus.
According to research, let’s look at additional techniques to enhance sleep.
Recommendations
- Ideal Room Temperature: Keep your room around 65 degrees Fahrenheit for restful sleep. A cool room supports your body’s natural temperature drop during sleep, aiding in a healthy sleep cycle and recovery.
- Nasal Strips for Easier Breathing: Products like Breathe Right strips can improve airflow, reduce congestion, and even offer calming scents like lavender, leading to better sleep.
- Humidifier Benefits: Increasing room moisture with a humidifier can open airways, potentially improving sleep quality. They’re especially useful in dry environments and can help with morning sore throats.
- White Noise for Sleep Continuity: White noise masks disruptive sounds, aiding in falling and staying asleep. There are various sound options, including rain and ocean, with apps available to turn off the noise automatically after you fall asleep.
- Allay Lamp for Comfortable Lighting: The Allay lamp, designed to emit a narrow band of green light, minimizes light sensitivity and promotes relaxation. It’s a good alternative to white light for pre-sleep reading.
- Limit Screen Time for Better Sleep: Excessive screen time can disrupt your body’s natural sleep cycle. Reducing screen usage, especially in the evening, can enhance melatonin production and improve sleep quality, aiding in healing.
- Weighted Blankets for Comfort: Weighing around 15 lbs, weighted blankets can decrease anxiety and pain perception, enhancing sleep quality. While research is limited, many users report significant sleep improvements.
Common Post-op Complications
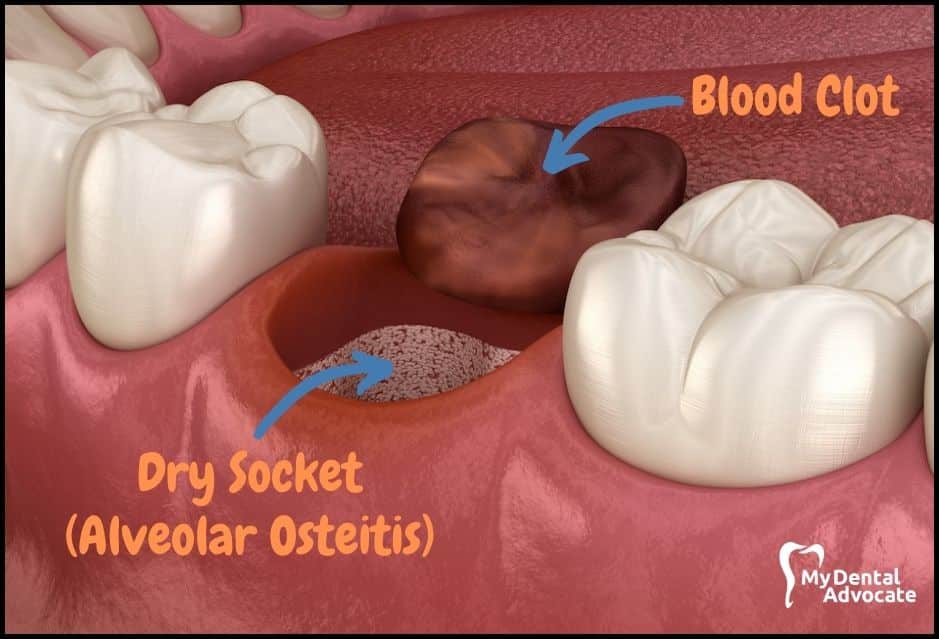
- Dry Socket Prevention and Treatment: Dry socket, a common issue where the blood clot is dislodged, exposes the bone and can be very painful. It typically happens around days 3 to 4. Treatment involves applying a special paste or irrigating with saline to encourage new clot formation.
- Managing Post-Operative Pain: Pain relief might include prescribed medications like Vicodin or Codeine. For those avoiding prescription drugs, combining 600 mg of Ibuprofen with 325 mg of Tylenol every 4-6 hours is effective. An ice pack can also help reduce pain, swelling, and inflammation.
- Paresthesia: Temporary or Permanent Numbness: This condition can happen if the inferior alveolar nerve (IAN), close to lower wisdom teeth, is traumatized during surgery. Recent studies show that IAN paresthesia occurs in about 0.35% to 8.4% of cases. While these percentages are low, they are important for both patients and dentists to consider.
Complete recovery of inferior alveolar nerve injury (IANI) occurs 6 to 8 weeks after the trauma, although it may take up to 24 months.
- Excessive Bleeding: Bleeding is normal up to 24 hours post-surgery. If it continues actively after 24 hours, especially for those on blood thinners, contact your dentist. A temporary solution is to bite on a tea bag.
- Risk of Damage to Adjacent Teeth: The force used in wisdom teeth removal can sometimes inadvertently damage nearby teeth, crowns, or fillings. Most such issues are quickly fixable by your dentist.
- TMJ Issues: The procedure may stretch and stress the TMJ, potentially causing clicking or popping sounds. If there’s no pain, it’s usually not a concern.
- Jaw Muscle Strain: The jaw muscles are stretched during surgery, leading to soreness or stiffness for 1-2 weeks. Use a cold compress initially, then alternate with warm packs. Limited jaw opening post-surgery is also common.
- Swelling and Infection: Swelling and bruising are expected, but signs of infection like elevated temperature need immediate attention, possibly requiring antibiotics. Use over-the-counter anti-inflammatories for pain and inflammation.
- Importance of Good Nutrition: Stay hydrated and eat a balanced diet of soft foods like macaroni & cheese, applesauce, and protein shakes. Poor nutrition can hinder healing and immune response. Adequate sleep is also crucial for recovery.
- Managing Nausea and Vomiting: Nausea may result from anesthesia or swallowing blood. Eat before bed, sip water at night, and take pain medications with food to prevent it. If nausea persists, especially after taking prescription pain meds, contact your dental office for advice.
Aftercare Instructions

- Take prescribed medication before the local anesthesia wears off
- Rest and recover for the first 3-4 days to allow the mouth to heal
- Avoid sucking, spitting, smoking or vigorously swishing to prevent dry socket.
- Use cold compress up to 36 hours after surgery to reduce inflammation, pain and swelling
- Alternate between hot and cold packs after that to stimulate healing
- Gently rinse mouth out with warm salt water 2-3x/day
- Gently massage TMJ and jaw muscles to decrease soreness
- Keep head elevated up to 72 hours after surgery to minimize pain and swelling
- Sleep often and stay off of your feet
- Avoid physical activity for 3-4 days
- Consume adequate amounts of fluid and electrolytes (Gatorade)
- Consume sufficient amounts of nutrients (soft-food diet)
Best/Worst Foods for Sleep & Recovery
Your oral surgeon will advise you to stay on a soft-food diet for 1-2 weeks. The diet allows time for your mouth, jaw muscles and gums to heal. A change in diet after wisdom tooth extraction can prevent you from getting adequate nutrients and disturb your sleep cycle.
Recommended Reading: 101 Foods to Eat After Dental Surgery, Implants or Wisdom Teeth RemovalSome foods are packed with crucial vitamins and minerals, while others will leave you sluggish and run down. Consider your body an engine that needs the right fuel to run efficiently.
Similar to the body, if certain food chemicals interact with the brain, it can lead to a positive or negative response.
Let’s explore the differences between certain foods and how they affect sleep and recovery.
Best Foods
- Kiwi: Eating kiwis before bed can help you fall asleep faster and improve sleep quality. They’re soft, easy to chew, and won’t disturb healing sockets. Plus, kiwis are rich in Vitamins C & E and potassium, which are great for recovery.
- Fatty Fish: Studies show fatty fish like salmon, rich in vitamin D and omega-3 fatty acids, enhance sleep quality and daytime function. These nutrients help regulate serotonin, aiding in sleep.
- Dairy: Milk contains melatonin and essential vitamins, making it beneficial for sleep. It’s also a good source of probiotics, which can ease gastrointestinal discomfort from medications. Night-milked dairy has more melatonin. Dairy products are also soft and soothing for a sore mouth.
Worst Foods
- Caffeine: Avoid caffeine in the afternoon and before bed. It can slow down wound healing and disrupt sleep. Stick to morning coffee if you need it.
- Alcohol: Skip alcohol while healing. It messes with your brain’s functions and sleep patterns, slowing down recovery.
- Nuts: Nuts are nutritious but risky after dental procedures. They can get stuck in tooth sockets, disrupting healing. Wait two weeks before enjoying nuts again.
My Experience & Expertise
Restful sleep affects our day and is essential for living a quality life.
After wisdom teeth removal, it’s vital to maintain a healthy sleep schedule to provide the best opportunity for healing and recovery.
Apply the sleeping tips and other helpful nutrition information to get back on your feet and on with your life.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!
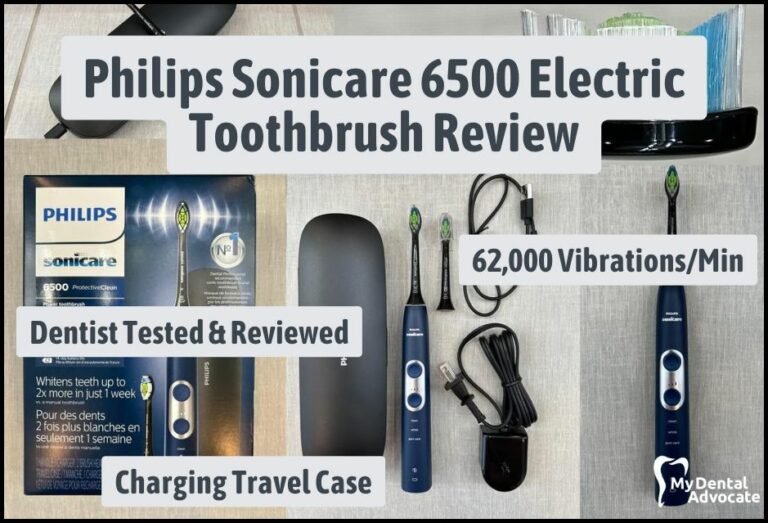
Philips Sonicare 6500 Electric Toothbrush Review 2024
In the realm of dental care, the Philips Sonicare 6500 Electric Toothbrush emerges as a revolutionary player. This cutting-edge device transcends standard cleaning, delivering a superior brushing experience that rewards you with a rejuvenated and sparkling smile.

Top 10 Habits for Improved Oral Health 2024
Have you ever visited the dentist anticipating an excellent report, only to question how much you floss? That would be a sinking feeling, especially if you thought you were doing a great job brushing and flossing. It may take some…

Oral-B Pro 1000 vs. Philips Sonicare 1100 Electric Toothbrush Review 2024
Seeking the best budget electric toothbrush? The Oral-B 1000 and Sonicare 1100 Electric Toothbrush are top contenders. We’ll position these two against each other, examine their features, analyze their performance, and finally, give you a solid recommendation.
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!