Pediatric Dental Sedation (Helpful Guide)
According to recent studies, 10%–20% of the US population avoid necessary dental care because of dental anxiety.
What’s scary is dental anxiety develops in childhood as a result of frightening and painful dental experiences.
In fact, 100,000–250,000 pediatric dental sedations are performed yearly in the USA.
Typical questions that you should address include: Is it safe? What are the risks my child doesn’t wake up? Let’s take a closer look at pediatric dental sedation from a dentist’s perspective.
Need Dental Advice? Ask Dr. Hannan!
What Is Pediatric Dental Sedation?
Pediatric dental sedation aims to reduce the child’s anxiety so they are calm and comfortable during the procedure. In addition, dental sedation (anesthesia) allows the child to relax and concentrate on the dentist’s instructions (if minimal sedation is used).
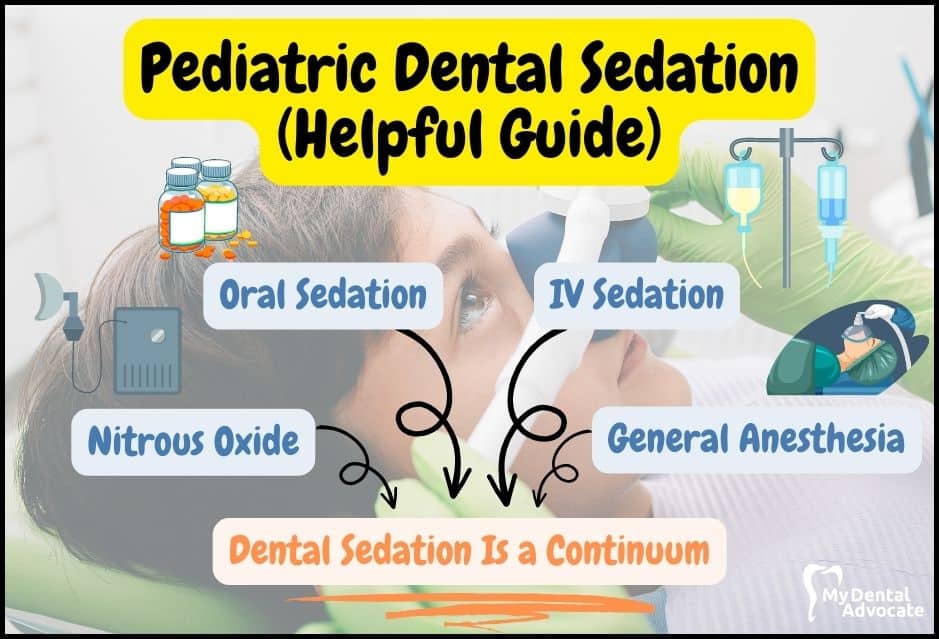
Recommended Reading: What is a Pediatric Dentist? (Read this FIRST)Alternatively, deep sedation medication or general anesthesia allows for unimpeded work. To achieve adequate dental sedation, the dentist will use one or more techniques: nitrous oxide, oral sedation, IV sedation and general anesthesia.
Numerous cavities, challenging behavior, and parent expectations support a need for sedation in pediatric dentistry.
Without anesthesia/sedation, the child and provider could be unsafe, leading to injury or harm.
Does My Child Need Dental Sedation?
Developing children lack the coping skills necessary to navigate the dental experience, occasionally making dentistry difficult.
While tooth decay can contribute to pain, additional issues can arise because of a cavity. For example, poor sleep diminishes attention, and difficulty learning can occur secondarily.
There are many reasons why your child needs pediatric dental sedation.
Common Reasons
- Pain Management: Kids often fear dental work, leading to anxiety and discomfort. Sedation helps prevent injury and eases their distress.
- Fear of Dentistry: Common fears include needles, loud noises, and separation from parents. Sedation helps alleviate these fears and anxieties.
- Difficulty Concentrating: Children may struggle to follow instructions, like keeping their mouth open, during procedures. Sedation aids in keeping them calm and cooperative.
- Uncomfortable Environment: Bright lights and noise in dental offices can overwhelm kids, causing nervousness and distraction. Sedation helps maintain their focus.
- Unpredictable Behavior: Kids may act out or struggle with situational awareness. Sedation can help manage these behaviors.
- Poor Self-Control: Children lacking self-control may interfere with the procedure. Sedation assists in ensuring cooperation and safety.
- Special Needs Considerations: For children with special needs or medical conditions, sedation may be necessary for a safe and successful treatment.
- Extensive Cavities: Sedation allows for comprehensive treatment in one visit, reducing the need for multiple appointments and associated anxiety.
What Are the Different Types of Dental Sedation?
Dental sedation is a continuum. Oral sedation is the most popular route of administration among pediatric dentists.
However, the taste can be bitter for children, and it’s not uncommon for children to spit it out. IV sedation is an alternative method, but placement of the intravenous cannula can be traumatic.
Recommended Reading: Silver Diamine Fluoride Treatment (What’s Involved?)One alternative is the transmucosal (intranasal, sublingual, buccal) route. The benefits of this route include direct absorption of drugs into the systemic circulation, avoiding metabolism and faster onset compared with oral sedation.
Transmucosal administration also results in less discomfort and better patient acceptance than intravenous sedation. But first, let’s look at the different dental sedation methods.
Dental Sedation Methods
- Nitrous Oxide Sedation: Laughing gas, a minimal sedation method, is used for minor dental procedures. It creates a feeling of heaviness and calmness, with potential side effects like nausea. The child remains responsive to cues.
- Oral Sedation: A moderate sedation, taken orally based on the child’s weight. It takes effect quickly, lasting about 30-60 minutes. Agents like benzodiazepines are used. It’s more challenging to control than IV or general anesthesia.
- IV Sedation: Deep sedation administered intravenously, suitable for children with complex medical needs or extensive dental work. It’s quicker and easier to manage than oral sedatives. Reversal agents are used post-treatment, with close monitoring of vital signs.
- General Anesthesia: Used for extensive procedures or high-risk cases in hospitals. It renders the child unconscious with no memory of the procedure. Post-treatment, the child may experience altered sensations. Vital signs are closely monitored until clearance for discharge.
Intranasal Sedation Administration
According to research, midazolam’s intranasal administration has proven to be a safe and effective sedative for quick procedures.
Along with rapid onset, a relatively speedy recovery has also been observed. Another advantage is that strict adherence to fasting requirements is not essential.
In addition, according to clinical trials, children sedated with intranasal midazolam had less risk of nausea, vomiting, and breathing complications.
Although intranasal administration is usually straightforward, relatively painless, and requires less patient cooperation, it has been associated with mucosal irritation.

Is Dental Sedation Safe for Children?
Dental sedation is considered safe if a complete medical history is taken, clinician competency is recognized, and standard of care is observed.
Unfortunately, in recent years, dental sedation has been responsible for a disproportionate number of cases that resulted in death or permanent brain damage.
Young children with more complex medical conditions appear at the most significant risk.
Recommended Reading: Stainless Steel Crowns (Pros & Cons)However, implementing simulation training and improvements in patient monitoring, including carbon dioxide measurements, are becoming a new standard of care. In addition, appropriate case selection and medication dosing (especially for overweight children) are also paramount.
Does Sedation Have Adverse Effects on the Brain?
Although there have been many positive developments in dental sedation medications and technology, it is believed that drugs used in sedation and anesthesia may have adverse effects on the developing brain.
In fact, initial research conducted on young animals’ brains demonstrated harm to young animals’ brains. Following the publication of these findings, researchers initiated human studies.
However, the results have revealed conflicting conclusions, with some showing long-term deficits in learning and behavior while others have not.
Results are difficult to assess as adverse neurologic outcomes are tricky to recognize and measure. Further investigation into these findings continues. While it will likely be many years before we understand sedation and anesthesia drugs, providers must be familiar with them.
Parents should be informed and weigh the pros and cons of dental sedation. In addition, dental sedation should only be indicated when a significant benefit to the child can be expected.
Benefits
According to a recent survey, over the past 30 years, parents have become much more accepting of general anesthesia for dental treatment.
With general anesthesia, minimal, moderate and deep sedation effectively facilitates a successful treatment case. In addition, there are many benefits of pediatric dental sedation.
Key Benefits
- Reduced Pain: Dental sedation helps prevent pain during treatment, ensuring the child remains still and cooperative. Many sedatives also induce amnesia, so the child won’t remember the procedure.
- Improved Cooperation: Sedation can ease anxiety, leading to better behavior and cooperation during dental visits, allowing the dentist to work more efficiently.
- Increased Safety: With close monitoring and advanced anesthesia training, sedation in dental clinics is safe. Vital signs like blood oxygen, blood pressure, and pulse are closely watched.
- Decreased Stress: Sedation helps manage anxiety and fear, reducing stress responses like increased heart rate and tension, ensuring a calm and relaxed experience for the child.
Risks
There is limited data on the mortality and morbidity induced by anesthesia and sedation in pediatric dental procedures.
According to previous studies, the highest mortality rate is observed in 2- to 5-year-old children in office-based dentistry operations with untrained team members.
Children younger than six are more susceptible to life-threatening complications, including apnea, airway obstruction, bronchospasm, and laryngospasm.
Recommended Reading: Fluoride Varnish vs. Fluoride Treatment (What’s the difference?)However, deep sedation with #propofol is a suitable technique with a high success rate for dental procedures in children. Researchers also concluded that a skilled anesthetist’s presence and a close monitoring process are required in pediatric dental procedures.
Lastly, the presence of a dentist anesthesiologist for providing office-based sedation is an emerging trend in the United States of America and should prevent complications.
Frequently Asked Questions (FAQ)
My Experience & Expertise
Many factors, including past experiences or fear of the unknown can induce children’s level of anxiety.
Pediatric dentistry has dramatically advanced over the years, and now many sedation options are available to manage the most medically complex child.
Sedation guidelines and best practices are available; talk to your pediatric dentist if you have any questions or concerns.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!
Sources
- Nelson TM, Xu Z. Pediatric dental sedation: challenges and opportunities. Clin Cosmet Investig Dent. 2015 Aug 26;7:97-106. doi: 10.2147/CCIDE.S64250. PMID: 26345425; PMCID: PMC4555969.
- Committee on Quality Management and Departmental Administration. Continuum of Depth of Sedation. American Society of Anesthesiologists. 2019.
- Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876–882.
- Razavi SS, Malekianzadeh B. The Efficacy and Complications of Deep Sedation in Pediatric Dental Patients: A Retrospective Cohort Study. Anesthesiol Res Pract. 2022 Jun 22;2022:5259283. doi: 10.1155/2022/5259283. PMID: 35783546; PMCID: PMC9242812.

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!

Baby Teething (Signs, Symptoms & Solutions)
Irritable babies drooling excessively and gnawing on their hands may be teething. Teething occurs when baby teeth erupt and can be uncomfortable for little ones. In addition, it can be incredibly stressful for parents and caregivers…
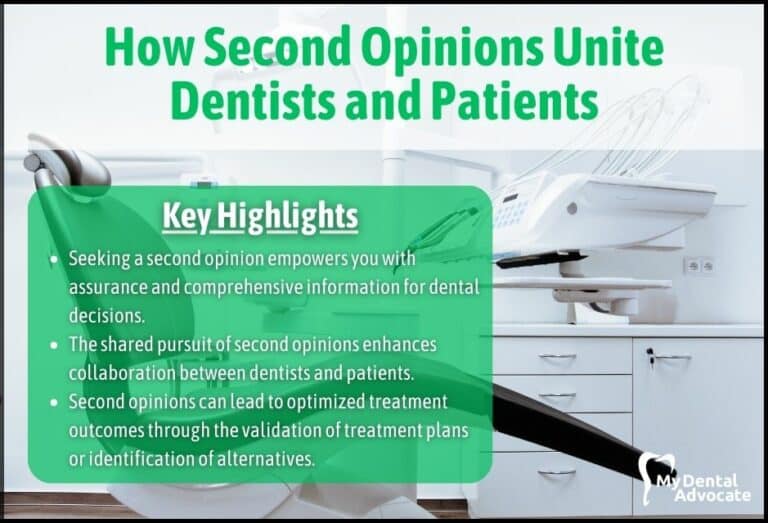
How Second Opinions Unite Dentists and Patients (Building Trust and Collaboration)
How Second Opinions Unite Dentists and Patients (Building Trust and Collaboration) Seeking input from another dental professional provides reassurance, promotes informed…
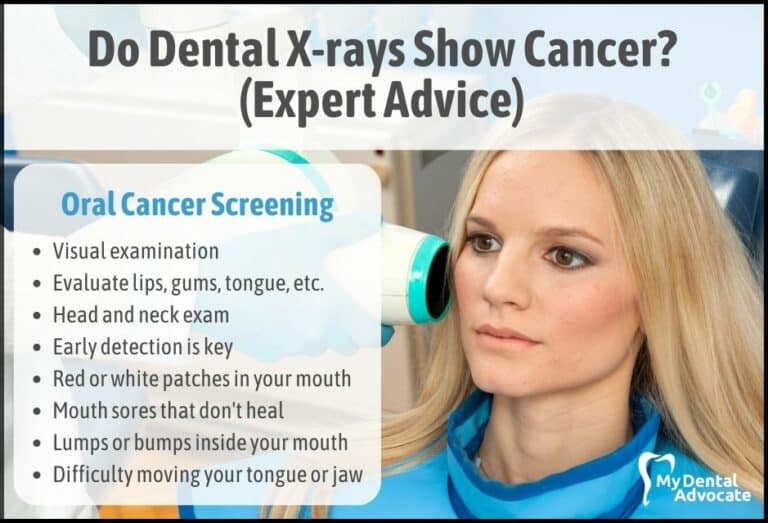
Do Dental X-rays Show Cancer? (Expert Advice)
When we step into a dental office for a routine checkup, one of the common procedures we encounter is the dental X-ray. Often, these X-rays are taken to help dentists identify hidden dental abnormalities, cavities, or gum disease.
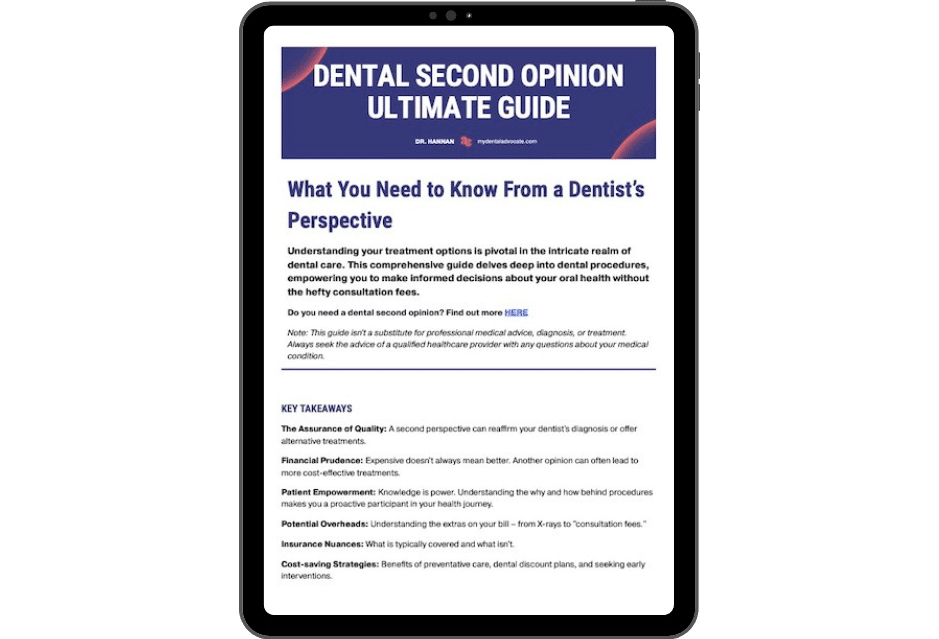
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!