Silver Diamine Fluoride Treatment (What’s Involved?)

According to the CDC, cavities are one of the greatest unmet dental needs. Did you know half of all children have had or will have a cavity?
Unfortunately, filling a cavity is a process that requires time out of your schedule and is costly.
Silver diamine fluoride treatment can arrest (stop) a cavity from progressing. This magic-like liquid is available at most dental offices.
Recommended Reading: Pediatric Dentistry | The Ultimate GuideNeed Dental Advice? Ask Dr. Hannan!
What Is Silver Diamine Fluoride (SDF)?
Silver diamine fluoride (SDF) is an FDA-approved, clear, cavity-arresting liquid that combines the antibacterial effects of silver and the remineralizing effects of fluoride.
According to multiple research articles, SDF is a promising therapeutic agent for managing cavities in young children and those with special care needs. It is specifically used to stop active tooth decay and prevent disease progression.
Did you know that silver diamine fluoride (SDF) has only recently become available in the United States?
Sodium diamine fluoride is revolutionary because it treats tooth decay with noninvasive methods and without numbing medication. However, SDF will not eliminate the need for restorative dentistry to repair moderate to severe decay.
In addition, it will not regrow lost enamel from tooth decay.
SDF has been used extensively worldwide for decades; however, it was approved by the FDA in 2014.
What’s interesting is the FDA-approved SDF is indicated for dentin sensitivity. Dentists primarily use it to treat and arrest small cavities, considered “off-label.”

How Does SDF Work?
According to up-to-date clinical research, the fluoride component strengthens the compromised tooth structure due to acid byproducts of bacterial metabolism.
In addition, SDF interferes with the bacteria biofilm, killing bacteria and causing damage (demineralization).
SDF disrupts the bacteria cavity-causing process on the tooth while enhancing demineralization (healing).
Silver’s antibacterial properties have been utilized to control infections for centuries, and its low toxicity makes it ideal for humans.
Fluoride is a mineral from the earth, and most drinking tap water naturally has some level of fluoride. However, some municipalities, towns and cities add more fluoride to the water as a public health measure.
Fluoride significantly increases the rate at which tooth enamel can be remineralized by saliva and strengthens the enamel’s resistance to harmful acids.
In addition, fluoride also has antimicrobial properties, killing bacteria in the mouth that cause cavities. According to a recent article, fluoride toothpaste prevents cavities worldwide – As much as a 15–30% decrease in cavity formation.
SDF is sometimes reported to have a slightly metallic taste during treatment.
How Is SDF Used?
I rarely used sodium diamine fluoride as a general dentist because we didn’t treat many kids. However, SDF is commonly used at pediatric dental offices. The pediatric dentist or dental assistant will isolate the tooth from contaminants.
Next, the dentist will use a small brush to apply it only on the affected areas. It’s applied one drop at a time and left undisturbed for about two minutes. It’s incredibly quick and painless!
Did you know that the silver diamine fluoride formula is 38% silver fluoride salt, which is water-soluble by adding ammonia?
Because SDF is water-soluble, it’s easily painted onto affected teeth in seconds.
Dentists generally only use SDF on baby teeth because it dyes the affected tooth structure a black or brown color. To read more about the application process, check out the SDF Chairside Guide by the American Academy of Pediatric Dentistry (AAPD).
SDF is prone to stain everything it touches, so care should be taken during the application procedure.
In addition, the tooth structure should be cleaned and free of plaque, food and other debris. Vaseline can be applied to lips and gums to protect against unwanted staining.
Recommended Reading: Pediatric Dental Sedation (Helpful Guide)Effectiveness & Application
According to the AAPD, SDF effectiveness in arresting (stopping) cavity lesions ranges from 47-90% after just one application, depending on the size and location of the cavity.
Front teeth have a higher chance of success compared to back teeth.
Recommended Reading: Fluoride Varnish vs. Fluoride Treatment (What’s the difference?)Benefits
If your child has a difficult time tolerating drilling at a young age, SDF could be a fantastic treatment.
Or, if your child has special health care needs that make it difficult to understand and cooperate during dental treatment, SDF would be helpful.
Remember that SDF is primarily used on baby teeth and is a great way to avoid needles and drilling while protecting your child against a spreading infection. In contrast, if your child has moderate to severe tooth decay already causing pain, SDF is not the best treatment.

Benefits of SDF
- Arrests cavities
- Prevents pain & infection
- Prevents or delays dental treatment
- Noninvasive
- Pain-free application
- Simple application process
- Timely and efficient (2 mins)
Risks & Side Effects
The most common side effect of SDF is the decayed areas will stain black. However, a healthy tooth structure will not stain.
In addition, SDF may discolor dental fillings and crowns.
As mentioned earlier, it’s essential to protect lips and gum tissue with vasoline as SDF will leave a harmless, temporary brown stain that is not easily washed away. However, the stain will disappear in one to three weeks.
SDF Risks
- Gum irritation
- Metallic taste
- Black or brown tooth stain
- Messy application
- Further reapplication treatments
- No guarantee of treatment success
- Recommended on primary teeth
These side effects may not include all the possible situations the manufacturer reported. If you notice other effects, please contact your dentist as soon as possible. In addition, avoid using SDF if you have a silver allergy.
Keep in mind that SDF has less fluoride than one fluoride varnish application, which is also often used to prevent cavities.
Expectations After Treatment
After the initial treatment, it’s essential to follow up with the dentist in two to four weeks to confirm that the cavity has been arrested.
Reapplication of SDF may be indicated if the treated lesions do not appear arrested (dark and hard). In addition, additional SDF applications can be completed at subsequent recall appointments as needed.
The dentist will decide based on the color and hardness of the lesion or evidence of lesion progression.
When cavities are not restored after SDF therapy, biannual reapplication shows increased cavity arrest rates compared to a single application.
Frequently Asked Questions (FAQ)
My Experience & Expertise
Learning you have a cavity is a tough pill to swallow, especially for a child.
The good news is that if the cavity is localized in a baby tooth, sodium diamine fluoride (SDF) can kill the cavity-causing bacteria and prevent tooth decay from progressing. It’s a simple procedure that takes two minutes to complete without local anesthesia.
Talk to your dentist about this revolutionary cavity-killing treatment if you think your child has a cavity.
Need a second opinion? We can help! Learn more. Knowledge is power when cultivating healthy dental habits. The more informed you are, the better positioned you’ll be to prevent avoidable and potentially costly dental procedures for you and your family. Watch for future blog posts, where we’ll continue sharing important information, product reviews and practical advice!
Sources
- Crystal YO. Evidence-Based Dentistry Update on Silver Diamine Fluoride. Dent Clin North Am. 2019.
- Bansal A. Recent advancements in fluoride: A systematic review. J Int Soc Prev Community Dent. 2015.
- Chairside Guide: Silver Diamine Fluoride in the Management of Dental Caries Lesions. American Academy of Pediatric Dentistry (AAPD).
- Silver Diamine Fluoride. American Dental Association.
- Gao SS. Caries remineralization and arresting effect in children by professionally applied fluoride treatment – A systematic review. BMC Oral Health 2016.

About the Author
Dr. Matthew Hannan, also known as “Dr. Advocate,” is a board-certified dentist on a mission to provide accurate dental patient education. He attended Baylor University before completing dental school at UT Health San Antonio School of Dentistry. He now lives in Arizona with his beautiful wife and 4 kids. Dr. Hannan believes everyone should access easy-to-read dental resources with relevant, up-to-date dental research and insight to improve their oral health.
Connect with Dr. Hannan!
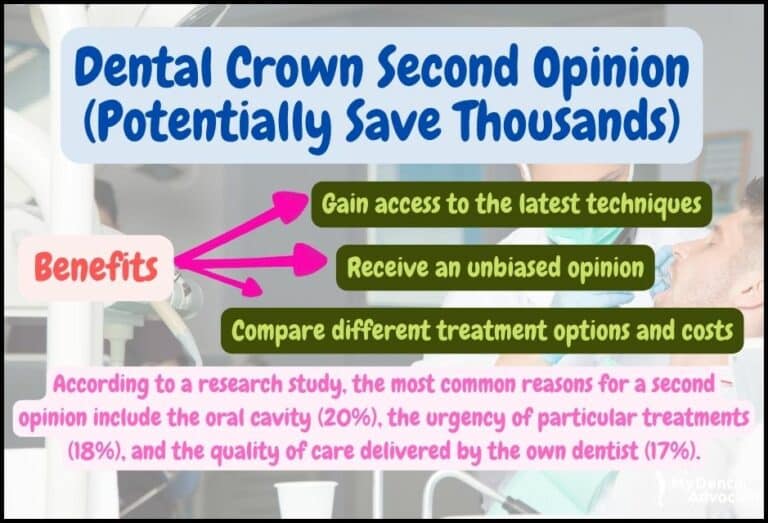
Dental Crown Second Opinion (Potentially Save Thousands)
I’ve seen hundreds of patients seeking a second opinion for dental work. In addition, statistics show that many patients have seen other dentists for a second opinion. When it comes to dental work, it is vital to ensure that you get the best care possible. Whether you need a dental crown…
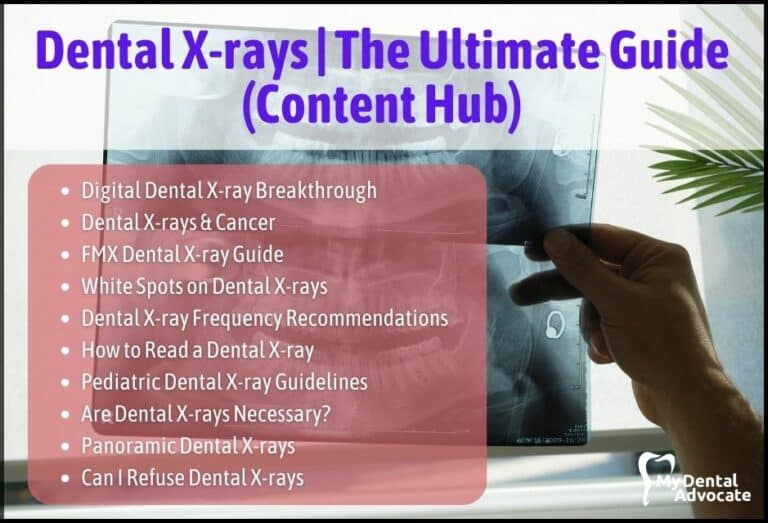
Dental X-rays | The Ultimate Guide (Content Hub)
In the vast realm of dentistry, one of the most revolutionary advancements has undoubtedly been the advent of dental X-rays. These powerful imaging tools have transformed how dental professionals diagnose, treat, and prevent oral conditions, granting a glimpse beneath the surface of the human mouth. This is the ultimate guide for dental X-rays. Below, you will find articles about dental X-rays from a dentist’s perspective.
What Are Primary Teeth? (Dentist Expert Thoughts)
One of the worst feelings for a parent is taking your child to the dentist for a routine cleaning only to find out that they have cavities.
You may find yourself wondering, “What went wrong? I thought we were doing a great job…
Gain Clarity with Our FREE Second Opinion Guide
Receive clear, expert second opinions online within 48 hours. Start today!
Product Reviews
Our 250+ dental product reviews (and counting), curated by an experienced dentist, are the most comprehensive online.
Toothbrush Genie
State-of-the-art chatbot designed to help you discover your perfect toothbrush in just a few simple steps!
Cavity Risk Assessment
Cutting-edge digital tool designed to evaluate your individual cavity risk based on your responses to a series of questions.
Gum Disease Assessment
Discover your gum disease risk with our quick and engaging 6-question assessment!